Translate this page into:
Cardiovascular Risk Assessment in Women with Psoriasis
*Corresponding author: Dr. Kalpana Medala, Department of Physiology, All India Institute of Medical Sciences, Hyderabad, Telangana, India. kalpsck@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Medala K, Taranikanti M, Umesh M, Gaur A, Vidya G, John NA. Cardiovascular Risk Assessment in Women with Psoriasis. Indian J Cardiovasc Dis Women. 2024;9:124-7. doi: 10.25259/IJCDW_67_2023
Abstract
Objectives:
Psoriasis is a chronic inflammatory skin disease. The exact cause of psoriasis is unclear; nevertheless, it is thought to be complex including several key components such as genetic predisposition, triggers from the environment, skin barrier disruption, and immunological dysfunction. About 85–90% of all psoriatic patients present with plaque type of psoriasis. The systemic nature of psoriasis makes an independent risk factor for cardiac disease. The main objective is to find the association between lipid profile, arterial stiffness, and psoriasis among female patients.
Materials and Methods:
Female patients with psoriasis in the age group of 20–50 years were selected. The duration of the study was 1 year. For lipid profile, after 12 h of fasting, 5 mL of blood was taken and analyzed by kit method using Transasia RX 1000. Low-density lipoprotein (LDL) cholesterol concentrations were estimated using the Friedewald formula. Arterial stiffness was measured using an oscillometric noninvasive arteriography. Right brachial ankle pulse wave velocity (RbaPWV), left brachial ankle pulse wave velocity (LbaPWV), and carotid femoral pulse wave velocity were measured in cm/s.
Results:
In the present study, 28% of the females were <38 years and 44% of females were in the range of 39–46 years. The mean value of cholesterol was (263.66 ± 47.74), Triglyceride (188.38 ± 27.56), high-density lipoprotein (HDL) (50.06 ± 18.05) LDL (171.60 ± 33.98), and very LDL (89.74 ± 13.361) mg/dL, respectively. Significant correlation was found between LbaPWV and Psoriasis (0.03), HDL and psoriasis (0.04), and psoriasis and RbaPWV (0.01).
Conclusion:
We conclude that psoriasis patients have hyperlipidemia, which will increase arterial stiffness and may lead to cardiovascular disorders (CVDs). Variables such as lipid profiles and arterial stiffness may be used as screening tools for the early detection of CVDs.
Keywords
Psoriasis
Lipid profile
Arterial stiffness
INTRODUCTION
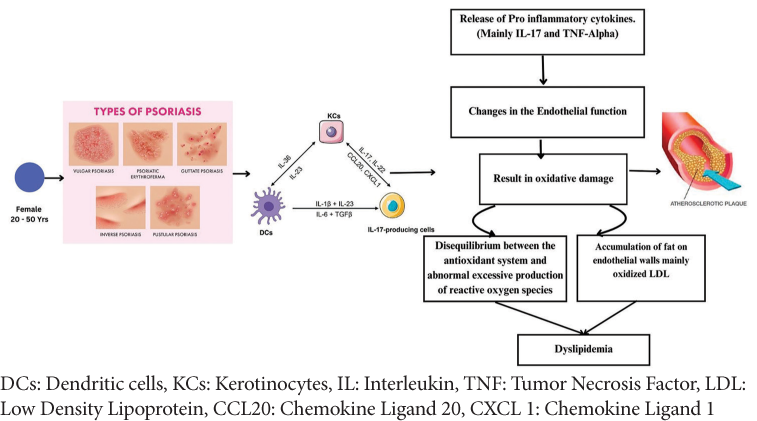
Psoriasis is a chronic inflammatory skin disease. It has a bimodal representation, one at the age of 20–30 years and the other peak at 50–60 years.[1] Erythematous, scaling lesions can form anywhere on the body, but they are most typically observed on the knees, elbows, scalp, and genitals.[2] The exact cause of psoriasis is unclear; nevertheless, it is thought to be complex including several key components such as genetic predisposition, triggers from the environment, skin barrier disruption, and immunological dysfunction.[3,4] About 85–90% of all psoriatic patients present with plaque type of psoriasis.[5] The systemic nature of psoriasis makes an independent risk factor for cardiac disease.[6] Dyslipidemia is 5 times higher in those psoriatic patients with severe cutaneous manifestations.[7] Psoriatic patients have lower high-density lipoprotein (HDL) levels, less HDL export capacity, and higher low-density lipoprotein (LDL) particle concentrations.[8] Psoriasis is characterized by neutrophil-derived myeloperoxidase, which drives lipoprotein oxidation and promotes damage both locally and systemically.[9,10] Supporting this idea, psoriasis patients have up to 30% more oxidized lipoprotein(a) and 15% more oxidized HDL than non-psoriasis patients. Several studies have shown that circulating lipids and lipid oxidization may play an important role to potentiate cardiovascular (CV) risk in psoriasis.[11] Clinically, these changes lead to a higher incidence of metabolic dysfunction, such as diabetes, as well as an increased risk of CV disease (CVD). Many studies have sought to identify the underlying processes that connect chronic inflammation and CV problems. Psoriasis causes complicated pathogenic interactions between the innate and adaptive immune systems. Risk of vascular disease was 2.2 times higher in 300 hospitalized patients with psoriasis than in controls with other dermatologic lesions. The estimated frequency of coronary heart disease in North American individuals with psoriasis is 14.3%, which is higher (11.3%) than in the overall population.[12,13] A cross-sectional study in Argentina found a significant connection between coronary artery disease and psoriasis, regardless of age, diabetes, hypertension, or smoking (odds ratio [OR] 1.48, 95% confidence interval [CI] 1.04–2.11, P = 0.03).[14] We hypothesize that despite lower CVD risk in women in general, women with psoriasis have a higher rate of cardiac stiffness and abnormal lipid profile which are predictors of CVD risk.
METHODOLOGY
This study was conducted at All India Institute of Medical Sciences (AIIMS) Bibinagar, Hyderabad, for a duration of 1 year. The study participants were recruited from the dermatology outpatient department. The female patients with psoriasis in the age group of 20–50 years were selected. The duration of the study was for 1 year. The study was approved by the Institute Ethics Committee (IEC Ref No: AIIMS/BBN/IEC/SEPT/2023/307 dated September 20, 2023). Written informed consent was obtained from all the study subjects. The consent was taken in local language. The subjects were explained about the purpose of the study and procedure of the study and were also explained about the risk involved in the study. For lipid profile, after 12 h of fasting, 5 mL of blood was taken and analyzed by kit method using Transasia RX 1000. LDL cholesterol concentrations were estimated using the Friedewald formula. Arterial stiffness was measured using an oscillometric noninvasive arteriography. This device uses 2 simple upper arm cuffs and 2 lower limb cuffs as a censor with cuff pressurized to at least 35 mm of Hg over actual systolic pressure. The device determines the right brachial ankle pulse wave velocity (RbaPWV), left brachial ankle pulse wave velocity (LbaPWV), and carotid femoral pulse wave velocity (PWV). Considering 14.3%, the prevalence of CVD in psoriasis, with 95% CI and 8% margin of error, sample size was estimated as 50.[12] All types of psoriasis (chronic plaque, palmoplantar, and erythrodermic) were included in the study. Diabetes mellitus, hypertension, menopause, thyroid disorders, obesity, women on oral contraceptive pills, and polycystic ovarian disease were excluded from the study.
Statistical analysis
Results on continuous measurements are presented as mean ± standard deviation and categorical measurements were presented as numbers or percentages. Data were analyzed using the Statistical Package for the Social Sciences version 25.0 (Statistical Package for the Social Sciences Inc., Chicago, IL, USA). Significance was assessed at 5% level of significance. Data were entered into Microsoft Excel versus 2019 and statistical analyses were performed using Chi-square test. P ≤ 0.05 was considered statistically significant.
RESULTS
In the present study, 28% (n = 14) of the females were <38 years and 44% (n = 22) in the age group of 39–46 years and above 28% (n = 14) of females were in the range of 47 years [Figure 1]. Among psoriasis arthropathy, palmoplantar psoriasis, and scalp psoriasis, the frequency of palmoplantar psoriasis was 44% (n = 22) [Figure 2]. The mean value of RbaPWV was 1739.32cm/s. The mean value of LbaPWV was 1958.72 cm/s. The mean value of cholesterol was (263.66 ± 47.74), triglyceride (188.38 ± 27.56), HDL (50.06 ± 18.05) LDL (171.60 ± 33.98), and very LDL (89.74 ± 13.361) mg/dL [Table 1]. Significant correlation was found between LbaPWV and psoriasis (0.03), HDL and psoriasis (0.04), and psoriasis and RbaPWV (0.01) [Table 2].
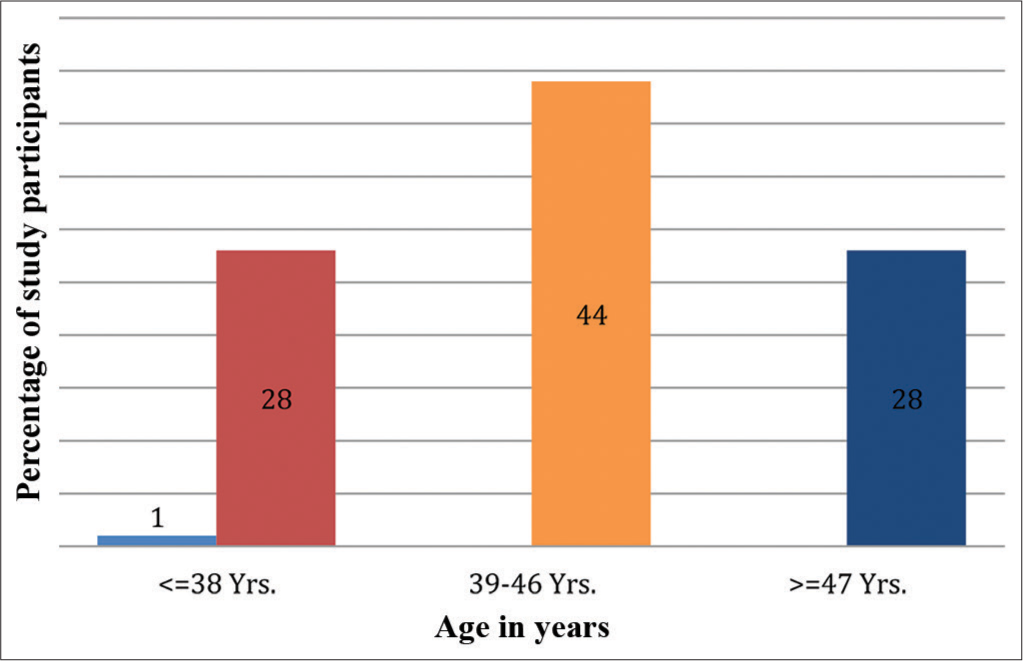
- Age-wise distribution of study population.
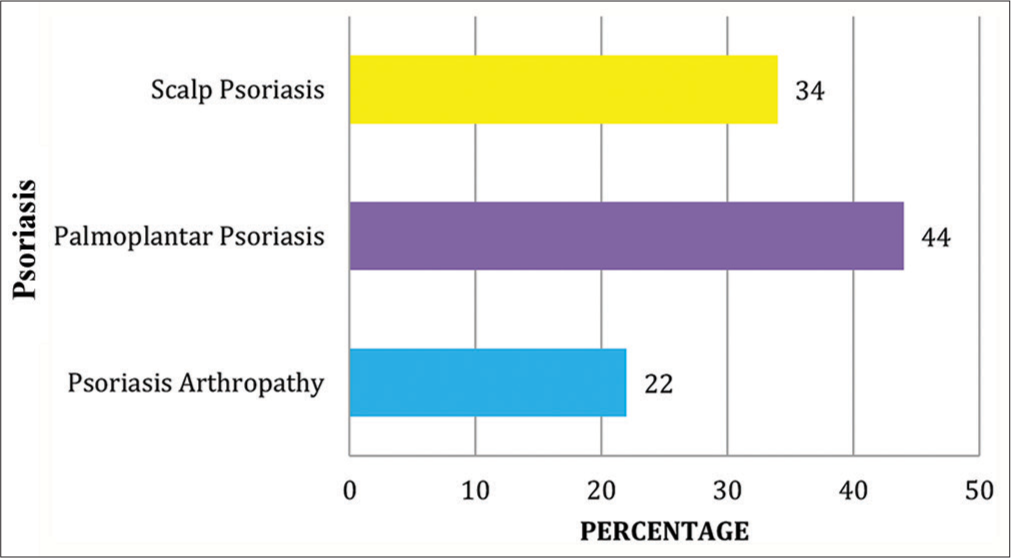
- Distribution of study population based on type of psoriasis.
| Category | N | Mean | Standard Deviation |
|---|---|---|---|
| Age | 50 | 43.46 | 8.029 |
| Height | 50 | 160.58 | 7.248 |
| Weight | 50 | 66.62 | 13.013 |
| RbaPWV | 50 | 1739.32 | 258.554 |
| LbaPWV | 50 | 1958.72 | 100.661 |
| CFPWV | 50 | 1373.22 | 305.731 |
| Cholesterol | 50 | 263.66 | 47.741 |
| Triglyceride | 50 | 188.38 | 27.564 |
| HDL | 50 | 50.06 | 18.055 |
| LDL | 50 | 171.60 | 33.987 |
| VLDL | 50 | 89.74 | 13.361 |
RabaPWV: Right brachial ankle pulse wave velocity, LbaPWV: Left brachial ankle pulse wave velocity, CFPWV: Carotid femoral pulse wave velocity, HDL: High-density lipoprotein, LDL: Low-density lipoprotein, VLDL: Very low-density lipoprotein
| S. No | Variables | R-value | P-value |
|---|---|---|---|
| 1. | RbaPWV cm/s | 0.359 | 0.01* |
| 2. | LbaPWV cm/s | 0.304 | 0.03* |
| 3. | HDL mg/dL | −0.291 | 0.04* |
| 4. | Cholesterol mg/dL | 0.302 | 0.03* |
| 5. | CFPWV cm/s | 0.302 | 0.03* |
DISCUSSION
In this present study, we were able to correlate between lipid profile and arterial stiffness among psoriatic female patients.
Psoriasis is a chronic skin disease that manifests as elevated, erythematous, and scaly plaques.[15] Inflammation caused by psoriasis may extend beyond the skin.[16] In this present study, we were able to correlate between lipid profile and arterial stiffness among psoriatic female patients. Psoriasis is a chronic skin disease that manifests as elevated, erythematous, and scaly plaques.[15] Inflammation caused by psoriasis may extend beyond the skin.[16] In this inflammatory skin lesion, many cytokines and chemokines are produced which has the systemic involvement which mainly targets the CV system. Psoriatic march was the terminology coined for this type of involvement. Boechat explained the link between psoriasis and CV system by his two plaques for one syndrome theory.[17]
Patients with psoriasis are more likely to develop CVD, a leading cause of morbidity and death in psoriasis patients.[18-20] Notably, increased ischemic CV risk in psoriasis patients appears to correlate with increased psoriasis activity. Indeed, severe psoriasis is linked with the highest CV risk (as compared to controls), including a thrice increased risk of myocardial infarction, and a 40% increased risk of CV-related mortality.[21,22] According to the literature, psoriasis has genetic and molecular linkages to atherosclerosis and other CV risk factors. The nonlinear and complex interaction of numerous stimuli regulating molecular pathways in various cell types is believed to contribute to the development of psoriasis and cardiovascular diseases (CVD). The study found that patients with psoriasis are prone to specific common genetic variants (HLA, FUT2, UBE2L3, and SH2B3) that increase the risk of dyslipidemia, hypertension, and CAD.[23] In our study, we found similar results in terms of lipid profile, primarily triglycerides, LDL, and very LDL. Dregan employed the stiffness index (SI) as a proxy diagnostic for subclinical atherosclerosis.[24] A photo plethysmograph transducer was attached to the participant’s dominant hand’s index finger and used to compute arterial SI. The SI was computed by dividing the participants’ height by the time between the first (systolic) and second (diastolic) wave peaks and was expressed in meters per second. SI is a clinical indicator of increased artery stiffness and has been shown to have a moderate connection with PWV, the gold standard measure of arterial stiffness.[25] A higher SI is supposed to signify stiffer arteries. Patients with psoriasis had higher mean SI values (9.49, 95% CI 9.36–9.61). Similar results were found in our study. This study concludes that patients with psoriasis have hyperlipidemia, which can increase arterial stiffness and contribute to CVD.
CONCLUSION
Early monitoring of the lipid profile and the arterial stiffness in the patients with psoriasis will act as a monitoring tool and prevent CVD in future.
Ethical approval
The study was approved by the Institute Ethics Committee (IEC Ref No: AIIMS/BBN/IEC/SEPT/2023/307 dated September 20, 2023).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
The present study is funded under PSS-2023 by WINCAR.
References
- Current Knowledge on Psoriasis and Autoimmune Diseases. Psoriasis Auckl NZ. 2016;6:7-32.
- [CrossRef] [PubMed] [Google Scholar]
- SciELO - Brazil - Diagnostic and Therapeutic Guidelines for Plaque Psoriasis - Brazilian Society. Available from: https://www.scielo.br/j/abd/a/wgprmjjzdxbqzgbzys8kdyj [Last accessed on 2023 Feb 14]
- [Google Scholar]
- Psoriasis Pathogenesis and Treatment. Int J Mol Sci. 2019;20:1475.
- [CrossRef] [PubMed] [Google Scholar]
- The Risk of Systemic Diseases in Those with Psoriasis and Psoriatic Arthritis: From Mechanisms to Clinic. Int J Mol Sci. 2020;21:7041.
- [CrossRef] [PubMed] [Google Scholar]
- Dyslipidemia in Psoriasis: A Case Controlled Study. Int Sch Res Notices. 2014;2014:729157.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis alters HDL composition and cholesterol efflux capacity. J Lipid Res. 2012;53:1618-24.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and Cardiovascular Disease: Novel Mechanisms and Evolving Therapeutics. Curr Atheroscler Rep. 2021;23:67.
- [CrossRef] [PubMed] [Google Scholar]
- Association Between Soluble Lectinlike Oxidized Low-Density Lipoprotein Receptor-1 and Coronary Artery Disease in Psoriasis. JAMA Dermatol. 2020;156:151-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dyslipidaemia and Oxidative Stress in Patients of Psoriasis: Emerging Cardiovascular Risk Factors. Indian J Med Res. 2017;146:708-13.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and Cardiovascular Risk: A Comprehensive Review. Adv Ther. 2020;37:2017-33.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary Artery Disease in Patients with Psoriasis. Medicina (B Aires). 2013;73:423-42.
- [Google Scholar]
- The Comorbid State of Psoriasis Patients in a University Dermatology Practice. J Dermatol Treat. 2005;16:319-23.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular Risk in Patients with Psoriasis: JACC Review Topic of the Week. J Am Coll Cardiol. 2021;77:1670-80.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriatic March, Skin Inflammation and Cardiovascular Events-Two Plaque for One Syndrome. Int J Cardiovasc Sci. 2020;33:109-11.
- [CrossRef] [Google Scholar]
- The Risk of Mortality in Patients with Psoriasis: Results from a Population-based Study. Arch Dermatol. 2007;143:1493-9.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of Major Cardiovascular Events in Patients with Psoriatic Arthritis, Psoriasis and Rheumatoid Arthritis: A Population-based Cohort Study. Ann Rheum Dis. 2015;74:326-32.
- [CrossRef] [PubMed] [Google Scholar]
- The “Psoriatic March”: A Concept of How Severe Psoriasis May Drive Cardiovascular Comorbidity. Exp Dermatol. 2011;20:303-7.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of Cardiovascular Disease in Individuals with Psoriasis: A Systematic Review and Meta-Analysis. J Invest Dermatol. 2013;133:2340-6.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and Cardiometabolic Diseases: Shared Genetic and Molecular Pathways. Int J Mol Sci. 2022;23:9063.
- [CrossRef] [PubMed] [Google Scholar]
- Association of Cardiovascular and Metabolic Disease Genes with Psoriasis. J Invest Dermatol. 2013;133:836-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arterial Stiffness Association with Chronic Inflammatory Disorders in the UK Biobank Study. Heart. 2018;104:1257-62.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of Central and Peripheral Arterial Stiffness: Studies Indicating the Need to Use a Combination of Techniques. Am J Hypertens. 2005;18:249-60.
- [CrossRef] [PubMed] [Google Scholar]








