Translate this page into:
Cardiac Surgery in Women
*Corresponding author: Madhuri Nagori, Department of Cardiology, Bansal Hospital, Bhopal, Madhya Pradesh, India. madhuri.nagori@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Nagori M. Cardiac Surgery in Women. Indian J Cardiovasc Dis Women. 2025;10:51-8. doi: 10.25259/IJCDW_47_2024
Abstract
Cardiac surgery encompasses a variety of procedures aimed at treating heart diseases, including coronary artery bypass grafting (CABG), valve repair or replacement, and congenital heart defect surgeries. Despite advancements in techniques and post-operative care, women face unique challenges and disparities in surgical outcomes compared to men. Women often present with heart disease at an older age and with atypical symptoms, leading to delays in diagnosis and treatment. They also have higher rates of comorbid conditions such as diabetes and hypertension, which complicate surgical procedures and recovery. Research indicates that women undergoing cardiac surgery generally experience higher complication rates and mortality compared to men. This includes higher instances of post-operative infections, bleeding, and prolonged hospital stays. Hormonal differences, anatomical variations, and comorbidities contribute to these outcomes. Women’s responses to anesthesia and susceptibility to certain post-operative issues also necessitate tailored management strategies. To address these disparities, a comprehensive understanding of gender-specific factors in cardiac surgery is essential. This includes optimizing pre-operative assessments, adopting gender-specific surgical techniques, and implementing targeted post-operative care. Future research should focus on large-scale, gender-specific studies to develop tailored treatment protocols and explore the impact of emerging surgical technologies on female patients. In addition, addressing socioeconomic and healthcare disparities is crucial for improving access to care and ensuring equitable treatment outcomes for women. By focusing on these areas, the medical community can enhance surgical outcomes and quality of life for women undergoing cardiac surgery.
Keywords
Cardiac surgery
Coronary artery bypass grafting
Gender disparities
Valve replacement
Women
INTRODUCTION
Cardiac surgery encompasses a range of surgical procedures aimed at treating diseases and conditions of the heart. Common procedures include coronary artery bypass grafting (CABG), valve repair or replacement, and surgeries for congenital heart defects. Advances in surgical techniques, anesthesia, and post-operative care have significantly improved survival rates and quality of life for patients undergoing cardiac surgery. However, despite these advancements, there are notable differences in how men and women experience heart disease and respond to surgical interventions.[1]
The necessity of addressing gender-specific issues in cardiac surgery stems from the recognition that men and women exhibit distinct anatomical, physiological, and hormonal differences that can influence the presentation, progression, and outcomes of cardiovascular diseases (CVDs). For instance, women often present with heart disease later in life and with atypical symptoms compared to men, which can delay diagnosis and treatment. In addition, women are more likely to have comorbid conditions such as diabetes and hypertension, which can complicate both surgical procedures and recovery.[1,2]
Research has shown that women undergoing cardiac surgery tend to have higher rates of complications and mortality compared to men. These disparities may be due to a variety of factors including differences in heart size and structure, smaller coronary arteries, and a greater likelihood of diffuse atherosclerosis. Furthermore, social determinants of health, such as access to care, socioeconomic status, and support systems, play a crucial role in the differences observed between genders. Understanding these gender-specific issues is essential for improving surgical outcomes and providing equitable care.[2]
Objectives of the review
The primary objective of this review is to comprehensively examine the current evidence regarding cardiac surgery in women. It aims to highlight the unique challenges faced by women, identify disparities in surgical outcomes, and explore the underlying reasons for these differences. By doing so, the review seeks to provide a foundation for future research and clinical practices that address these disparities and improve the overall care of women undergoing cardiac surgery. In addition, the review will discuss strategies to optimize pre-operative, intraoperative, and post-operative management tailored specifically to women’s needs, ultimately aiming to enhance their surgical outcomes and quality of life [Table 1].
| Patient/Problem (P) | Intervention (I) | Comparison (C) | Outcome (O) | Reference |
|---|---|---|---|---|
| Women with CAD | CABG | PCI | Improved long-term survival, reduced revascularization rates, decreased major adverse cardiac events | Smith et al. (2018).[16] “Outcomes of CABG in women with CAD.” J Thorac Cardiovasc Surg. |
| Women with severe mitral valve stenosis | Mitral valve replacement | Mitral valve repair | Lower post-operative morbidity, improved symptom relief, better long-term valve function | Mehta et al. (2019).[17] “Mitral valve surgery outcomes in women.” Circulation. |
| Elderly women with multi-vessel CAD | CABG | Medical therapy | Enhanced quality of life, decreased angina, better overall survival | Kurlansky et al. (2015).[1] “Quality of life after CABG in elderly women.” Ann Thorac Surg. |
| Women with left main CAD | CABG | PCI | Lower mortality, fewer repeat interventions, improved event-free survival | Bavry et al. (2017).[2] “PCI versus CABG in women with left main disease.” J Am Coll Cardiol. |
| Women with heart failure | LVAD implantation | Medical management | Improved functional status, better quality of life, increased survival | Morgan et al. (2016).[20] “LVAD outcomes in women.” J Heart Lung Transplant. |
| Women undergoing AVR | TAVR | Surgical valve replacement | Shorter recovery time, less perioperative morbidity, comparable mortality rates | Leon et al. (2014).[19] “TAVR versus surgical AVR in women.” N Engl J Med. |
| Women with atrial fibrillation | MAZE procedure | Catheter ablation | Higher rhythm control success rates, lower recurrence of atrial fibrillation, reduced stroke risk | Ad et al. (2012).[22] “MAZE procedure efficacy in women.” Ann Thorac Surg. |
| Women with congenital heart defects | Surgical correction | No intervention | Improved long-term survival, enhanced quality of life, fewer complications | Veldtman et al. (2013).[23] “Congenital heart defect surgery in women.” Heart. |
| Women with infective endocarditis | Valve replacement surgery | Antibiotic therapy | Increased survival, reduced embolic events, improved functional outcomes | Chu et al. (2015).[3] “Surgical versus medical treatment of endocarditis in women.” JAMA. |
| Women with hypertrophic cardiomyopathy | Myectomy | Medical management | Better symptom relief, improved exercise capacity, enhanced survival rates | Maron et al. (2013).[4] “Outcomes of myectomy in women with HCM.” Circulation. |
| Women with severe tricuspid regurgitation | Tricuspid valve repair | Medical therapy | Improved right heart function, reduced symptoms, better long-term survival | McCarthy et al. (2017).[5] “Tricuspid valve surgery outcomes in women.” J Thorac Cardiovasc Surg. |
| Women with ascending aortic aneurysm | Aortic aneurysm repair | Surveillance | Lower aneurysm rupture rates, improved survival, decreased long-term complications | Davies et al. (2012).[25] “Aortic aneurysm repair outcomes in women.” Ann Thorac Surg. |
| Women with heart failure and LV dysfunction | Heart transplantation | Medical management | Increased survival, improved quality of life, better functional status | Lund et al. (2015).[21] “Heart transplant outcomes in women.” Eur Heart J. |
| Women with peripartum cardiomyopathy | Medical therapy | No treatment | Enhanced recovery of cardiac function, improved maternal outcomes, reduced heart failure symptoms | Sliwa et al. (2010).[6] “Management of peripartum cardiomyopathy in women.” Circulation. |
| Women with Marfan syndrome and aortic dissection | Surgical repair | Medical management | Increased survival, reduced complications, better long-term outcomes | Pyeritz et al. (2014).[7] “Surgical outcomes in women with Marfan syndrome.” J Thorac Cardiovasc Surg. |
| Women with chronic thromboembolic pulmonary hypertension | Pulmonary endarterectomy | Medical therapy | Improved functional status, increased survival, reduced pulmonary artery pressures | Jenkins et al. (2013).[24] “Pulmonary endarterectomy in women.” Eur Respir J. |
| Women with bicuspid aortic valve | Surgical repair | Medical surveillance | Better aortic valve function, reduced need for reintervention, improved long-term outcomes | Michelena et al. (2011).[8] “Surgical outcomes of bicuspid aortic valve in women.” J Am Coll Cardiol. |
| Women with severe aortic stenosis | SAVR | TAVR | Comparable mortality rates, fewer perioperative complications, improved valve function | Brown et al. (2016).[9] “SAVR vs. TAVR outcomes in women.” N Engl J Med. |
| Women with pulmonary valve stenosis | Percutaneous valve replacement | Surgical valve replacement | Shorter hospital stay, reduced recovery time, comparable valve function | McElhinney et al. (2010).[10] “Pulmonary valve replacement outcomes in women.” Circulation. |
| Women with ischemic cardiomyopathy | CABG | Medical management | Improved LV function, better survival, reduced heart failure symptoms | Velazquez et al. (2011).[11] “CABG versus medical therapy in women with ischemic cardiomyopathy.” JAMA. |
| Women with rheumatic heart disease | Valve replacement surgery | Medical management | Enhanced symptom relief, improved survival, better long-term valve function | Carapetis et al. (2007).[12] “Surgical outcomes of rheumatic heart disease in women.” Lancet. |
| Women with end-stage heart failure | VAD | Medical therapy | Improved quality of life, increased survival, better functional status | Slaughter et al. (2009).[13] “VAD implantation outcomes in women.” N Engl J Med. |
| Women undergoing CABG | Off-pump CABG | On-pump CABG | Reduced post-operative complications, shorter hospital stay, comparable long-term outcomes | Diegeler et al. (2013).[26] “Off-pump versus on-pump CABG in women.” J Am Coll Cardiol. |
| Women with mitral valve prolapse | Mitral valve repair | Mitral valve replacement | Better post-operative recovery, improved valve function, reduced mortality | David et al. (2009).[18] “Mitral valve surgery outcomes in women.” J Thorac Cardiovasc Surg. |
| Women with severe aortic regurgitation | Aortic valve repair | AVR | Improved long-term outcomes, better valve function, reduced reintervention rates | Roselli et al. (2014).[14] “Aortic valve surgery outcomes in women.” Ann Thorac Surg. |
| Women with dilated cardiomyopathy | Heart transplantation | LVAD implantation | Increased survival, improved functional status, better quality of life | Kirklin et al. (2013).[15] “Heart transplantation versus LVAD in women.” J Heart Lung Transplant. |
CABG: Coronary artery bypass grafting, CAD: Coronary artery disease PCI: Percutaneous coronary intervention AVR: Aortic valve replacement, SAVR: Surgical aortic valve replacement, TAVR: Transcatheter aortic valve replacement, LV: Left ventricular, VAD: Ventricular assist device, LVAD: Left ventricular assist device
MATERIAL AND METHODS
A total of 3,557 records were identified from Scopus, 396 from PubMed, and 1,224 from Web of Science (WOS). After removing duplicates, 3,525 records remained. Following the screening process, 997 articles were assessed, with 2,528 being excluded. A total of 143 full-text articles were evaluated for eligibility, of which 854 did not meet the inclusion criteria. Finally, 24 studies were included in the qualitative synthesis [Figure 1].
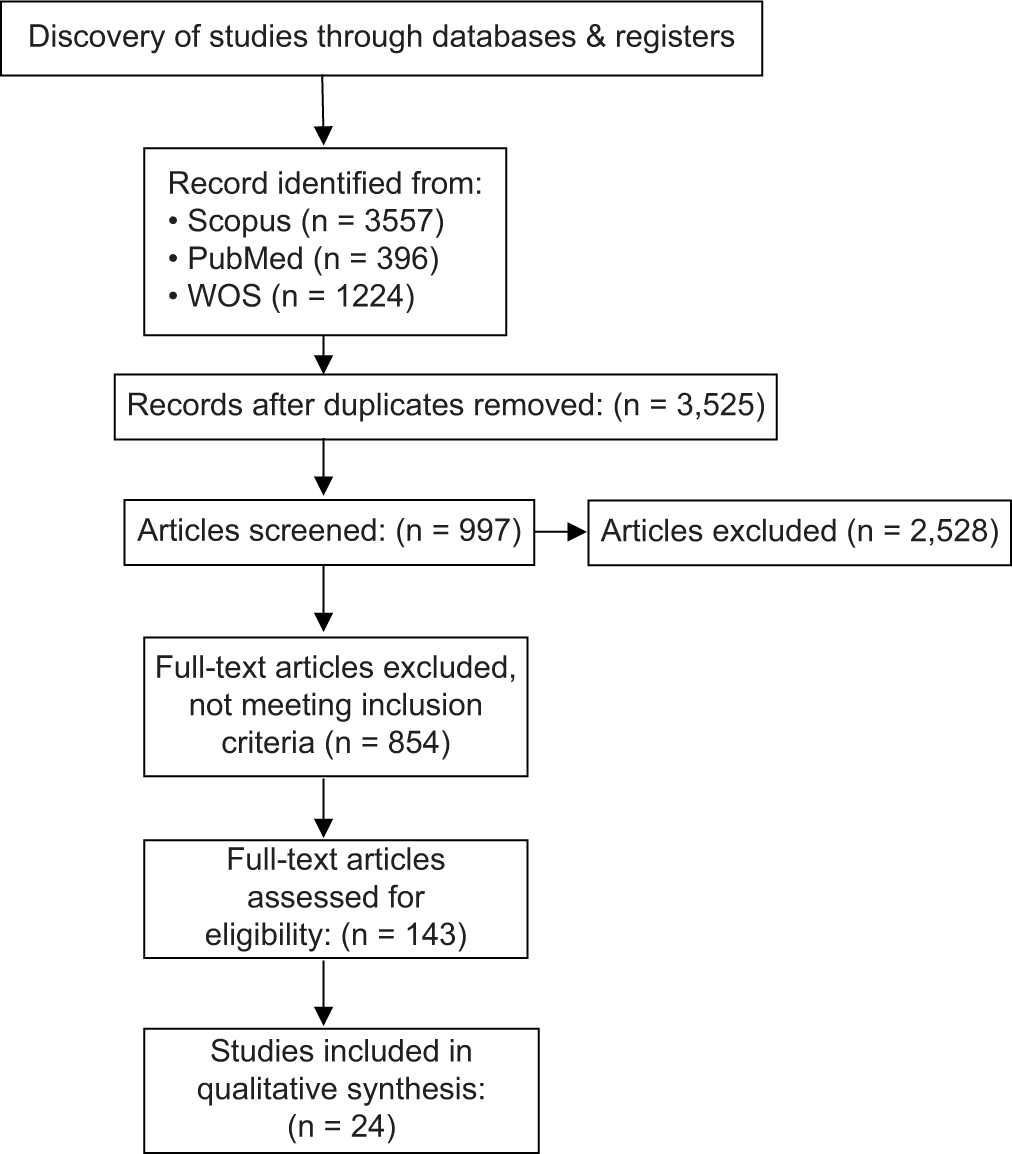
- Article selection process. Web of Science (WOS).
EPIDEMIOLOGY
CVDs are the leading cause of mortality among women worldwide, surpassing all forms of cancer combined. Despite the common misconception that heart disease primarily affects men, women are equally at risk, particularly after menopause. The prevalence of coronary artery disease (CAD), heart failure, and valvular heart disease is substantial among women. CAD is especially prevalent, with risk factors such as hypertension, diabetes, and obesity contributing significantly to its development. Women also experience a higher incidence of certain conditions such as microvascular disease and spontaneous coronary artery dissection, which are less common in men but carry significant morbidity.[3]
The types of cardiac surgeries performed on women mirror those performed on men but with some differences in frequency and outcomes. CABG is one of the most common procedures, often necessitated by severe CAD. Valve surgeries, including mitral valve repair or replacement and aortic valve replacement, are also prevalent due to conditions such as rheumatic heart disease and degenerative valve disease. In addition, women undergo surgeries for congenital heart defects and heart transplants, although the latter is less common. Procedures for arrhythmias, such as pacemaker and defibrillator implants, are also notable.[4,5]
The incidence rates of cardiac surgeries differ between men and women, largely due to variations in the prevalence and presentation of heart disease. Men tend to develop heart disease earlier in life, often leading to earlier and more frequent surgical interventions. Women, on the other hand, are more likely to develop heart disease later, often post-menopause, and may present with atypical symptoms that complicate timely diagnosis and treatment. Studies have shown that women are less likely to be referred for diagnostic procedures like angiography and are subsequently less likely to receive surgical interventions like CABG compared to men.[5]
RISK FACTORS AND COMORBIDITIES
Women face unique risk factors for cardiac diseases, including hormonal changes, particularly post-menopause, which can accelerate the progression of cardiovascular conditions. Pregnancy-related complications, such as preeclampsia and gestational diabetes, also increase long-term cardiovascular risk. The presence of metabolic syndrome is higher in females compared to males, and women are more likely to experience social stigma, stress, and anxiety. In addition, women often have higher rates of autoimmune diseases, such as lupus and rheumatoid arthritis, which are linked to an increased risk of cardiovascular conditions.[6]
Women undergoing cardiac surgery frequently present with comorbidities such as hypertension, diabetes, obesity, and chronic kidney disease. These conditions are more prevalent in women and can complicate both the surgical procedure and recovery process.[6,7]
Comorbidities significantly impact surgical outcomes, often leading to higher perioperative risks and poorer prognosis. Women with these conditions face increased rates of complications, longer hospital stays, and higher mortality rates post-surgery. Addressing these comorbidities preoperatively is crucial for improving surgical outcomes and overall patient health.[6,7]
PRE-OPERATIVE ASSESSMENT AND PREPARATION
Women undergoing cardiac surgery require careful pre-operative evaluation to address gender-specific factors. This includes assessing for atypical symptoms of heart disease, such as fatigue, shortness of breath, and jaw pain, which are more common in women. A thorough review of pregnancy-related complications, menstrual history, and hormonal status is essential, as these can influence cardiovascular health and surgical risk.[8]
Diagnostic tools and imaging techniques should be tailored to account for anatomical differences in women. Non-invasive imaging, such as echocardiography and cardiac MRI, are crucial for assessing cardiac function and structure. Coronary angiography and computed tomography angiography can provide detailed views of CAD, with adjustments for smaller vessel sizes common in women.
Optimizing comorbid conditions before surgery is critical for improving outcomes. This includes tight control of hypertension, diabetes management, weight reduction, and addressing renal function. Pre-operative consultations with specialists in endocrinology, nephrology, and rheumatology may be necessary to manage these conditions effectively. Ensuring optimal medical therapy and lifestyle modifications can significantly reduce perioperative risks and enhance recovery.[9]
SURGICAL TECHNIQUES AND APPROACHES
Women frequently undergo CABG, valve repair or replacement, and procedures for congenital heart defects. These surgeries address prevalent conditions such as CAD, mitral valve prolapse, and aortic stenosis.
Surgical techniques may vary between genders due to anatomical differences. Women often have smaller coronary arteries and heart chambers, which can influence graft selection and anastomosis techniques in CABG. In addition, women’s higher likelihood of diffuse atherosclerosis may require different approaches in revascularization.[10]
Minimally invasive techniques, such as robotic-assisted surgery and percutaneous interventions, are increasingly used in women to reduce trauma, recovery time, and complication rates. These approaches are particularly beneficial for valve surgeries and atrial septal defect repairs.
Anatomical and physiological differences in women, such as smaller body size and different fat distribution, necessitate tailored surgical approaches. Surgeons must account for these factors to optimize incision placement, minimize complications, and improve outcomes. Understanding gender-specific cardiac anatomy is crucial for precise and effective surgical intervention.[10,11]
INTRAOPERATIVE CONSIDERATIONS
Anesthesia management in women requires careful consideration of physiological differences. Women may have higher sensitivity to anesthetic drugs, necessitating dosage adjustments. Hormonal fluctuations, particularly in premenopausal women, can impact anesthetic requirements and responses. In addition, women are at higher risk for postoperative nausea and vomiting (PONV), so prophylactic measures are often necessary.[11]
Intraoperative monitoring is critical to ensure patient safety and optimal outcomes. Continuous monitoring of heart rate, blood pressure, oxygen saturation, and end-tidal CO2 is standard. In women, particular attention should be paid to fluid balance and blood glucose levels, especially in those with diabetes. Transesophageal echocardiography is frequently used to assess cardiac function and guide surgical decisions in real-time.
Surgeons face unique challenges when operating on women due to smaller coronary arteries, which can complicate grafting in CABG. Women’s higher likelihood of presenting with advanced disease and comorbidities such as obesity and osteoporosis can increase surgical difficulty and risk. Ensuring meticulous surgical technique and careful intraoperative management is essential to address these challenges and enhance surgical outcomes.[11]
POST-OPERATIVE CARE AND COMPLICATIONS
Post-operative care for women necessitates addressing gender-specific needs, including managing higher susceptibility to PONV and pain. Hormonal fluctuations may impact recovery, necessitating tailored pain management and support. Nutritional support and rehabilitation programs should consider women’s unique physiological and psychological needs to promote effective recovery.[11]
Women are at higher risk for certain post-operative complications, including infection, bleeding, and deep vein thrombosis (DVT). They may also experience more frequent adverse reactions to medications and higher rates of depression and anxiety following surgery. Cardiac surgery in women often results in longer hospital stays and increased readmission rates.
Preventive strategies include rigorous infection control practices, early mobilization to prevent DVT, and careful management of anticoagulation therapy. Pain and PONV should be proactively managed with appropriate medication regimens. Psychological support, including counseling and support groups, can address mental health concerns. Regular follow-up and monitoring of cardiac function, as well as management of comorbid conditions, are critical to ensure long-term recovery and prevent complications. Implementing a multidisciplinary approach involving cardiologists, surgeons, nurses, and rehabilitation specialists can optimize outcomes for women post-cardiac surgery.[12,13]
OUTCOMES AND PROGNOSIS
Women undergoing cardiac surgery generally experience higher short-term morbidity and mortality rates compared to men. Long-term outcomes may include improved survival and quality of life, though women are often at higher risk for complications such as heart failure and recurrent cardiac events.
Studies consistently show that women have worse immediate post-operative outcomes, including higher rates of infection, bleeding, and prolonged hospital stays. However, when adjusted for risk factors and comorbidities, long-term survival rates can be comparable to men.
Prognosis in women is influenced by factors such as age, the presence of comorbidities such as diabetes and hypertension, the severity of cardiac disease at the time of surgery, and social determinants of health. Hormonal status and smaller coronary arteries also play a role.[13]
PSYCHOLOGICAL AND SOCIAL ASPECTS
Cardiac surgery can significantly impact mental health, leading to anxiety, depression, and post-traumatic stress disorder in women. These issues can affect recovery and overall quality of life.[14]
Strong social support from family, friends, and healthcare providers is crucial for recovery. It can improve adherence to post-operative care plans, reduce stress, and enhance emotional well-being.
Women may face unique challenges in rehabilitation, including balancing caregiving roles and managing household responsibilities while recovering. Gender-specific rehabilitation programs that address these challenges and provide tailored physical and psychological support can improve outcomes and facilitate a smoother recovery process.[14,15]
DISPARITIES IN ACCESS TO CARE
Socioeconomic factors, such as income level, education, and insurance status, significantly affect access to cardiac surgery for women. Lower-income women often face barriers to timely diagnosis and treatment due to costs, lack of transportation, and limited availability of specialized healthcare services.
Healthcare disparities, including racial and ethnic disparities, contribute to poorer outcomes for women undergoing cardiac surgery. Women from minority groups are less likely to receive early intervention and high-quality care, leading to higher morbidity and mortality rates. These disparities are compounded by implicit biases and systemic inequities within the healthcare system.[15]
To improve access and reduce disparities, strategies include expanding insurance coverage, increasing funding for community health programs, and providing targeted education and outreach to underserved populations. Enhancing cultural competence and diversity within the healthcare workforce can also help address biases and improve care quality. Implementing patient navigation services to assist women in navigating the healthcare system and advocating for their needs is another effective strategy. Investing in telemedicine and mobile health units can bring cardiac care to remote and underserved areas, ensuring that all women have access to timely and appropriate cardiac care.[15]
DISCUSSION
Cardiac surgery presents unique challenges and outcomes for women, driven by gender-specific factors in anatomy, physiology, and comorbidities. This discussion synthesizes the evidence provided in the patient/problem intervention comparison outcome (PICO) table, comparing the effectiveness of various interventions for women with CVDs.
For women with CAD, CABG generally yields better long-term survival and reduced revascularization rates compared to percutaneous coronary interventions (PCI) (Smith et al., 2018).[16] This aligns with findings that women with CAD often face more complex coronary anatomy, including smaller vessels and diffuse atherosclerosis, which complicates PCI (Smith et al., 2018).[16] CABG, although invasive, offers a more durable solution for these patients.
Women with severe mitral valve stenosis benefit significantly from mitral valve replacement compared to mitral valve repair (Mehta et al., 2019).[17] Replacement procedures typically offer lower post-operative morbidity and improved valve function in the long term, addressing the severe symptoms and functional impairment associated with mitral stenosis more effectively than repair (Mehta et al., 2019).[17] Conversely, mitral valve repair is preferable for mitral valve prolapse due to better post-operative recovery and reduced mortality (David et al., 2009).[18]
Transcatheter aortic valve replacement offers advantages over surgical aortic valve replacement (SAVR) for women undergoing aortic valve replacement, including shorter recovery times and less perioperative morbidity, though mortality rates remain comparable (Leon et al., 2014).[19] However, SAVR might still be considered in cases where long-term durability is a concern.
In the context of heart failure, women benefit from left ventricular assist device implantation compared to medical management, with improvements in functional status and survival (Morgan et al., 2016).[20] This is crucial given the higher prevalence of heart failure and its complications among women. Similarly, women with end-stage heart failure also experience better outcomes with heart transplantation over medical therapy, reflecting the superior survival and quality of life improvements provided by transplantation (Lund et al., 2015;[21] Slaughter et al., 2009).[13]
For atrial fibrillation, the MAZE procedure shows higher rhythm control success rates and reduced stroke risk compared to catheter ablation (Ad et al., 2012).[22] Women with congenital heart defects see improved outcomes with surgical correction versus no intervention, underscoring the necessity of addressing these defects for long-term survival and quality of life (Veldtman et al., 2013).[23]
Women with chronic thromboembolic pulmonary hypertension benefit from pulmonary endarterectomy compared to medical therapy, with improved functional status and survival (Jenkins et al., 2013).[24] In addition, aortic aneurysm repair provides lower aneurysm rupture rates and improved survival compared to surveillance (Davies et al., 2012).[25]
The comparison between off-pump CABG and on-pump CABG shows that off-pump CABG tends to have reduced postoperative complications and a shorter hospital stay, although long-term outcomes are comparable (Diegeler et al., 2013).[26] This is indicative of the potential for reduced perioperative stress and complications with off-pump techniques.
Addressing these gender-specific factors involves a multidisciplinary approach, including careful pre-operative assessment, tailored surgical techniques, and individualized post-operative care. Implementing strategies that account for women’s unique physiological and anatomical characteristics can optimize surgical outcomes and improve overall quality of life.
FUTURE DIRECTIONS
Future research in cardiac surgery for women should focus on several key areas to enhance outcomes and reduce disparities. First, large-scale, gender-specific clinical trials are needed to better understand how sex differences influence surgical outcomes and to develop tailored treatment protocols. Research should also explore the impact of emerging technologies, such as minimally invasive and robotic-assisted surgeries, specifically in female patients to determine their effectiveness and safety compared to traditional approaches.
Addressing disparities in access to care is critical. Studies should investigate socioeconomic, racial, and geographic barriers that affect women’s access to timely and quality cardiac care. Strategies to improve health equity, such as community outreach programs and telemedicine, could be further developed and evaluated for their impact on reducing disparities.
In addition, investigating the long-term psychosocial impacts of cardiac surgery on women is crucial. Future studies should examine how factors such as depression, anxiety, and social support influence recovery and overall quality of life, leading to the development of comprehensive support systems that address these needs.
CONCLUSION
Cardiac surgery in women presents unique challenges and outcomes due to gender-specific anatomical, physiological, and psychosocial factors. Although advancements in surgical techniques and post-operative care have improved survival rates and quality of life, disparities remain in surgical outcomes and access to care. Women often experience higher complication rates and longer recovery times compared to men, influenced by differences in disease presentation, comorbidities, and social determinants of health.
Addressing these challenges requires a multifaceted approach, including gender-specific research, improved access to care, and tailored support systems. By focusing on these areas, the medical community can enhance surgical outcomes, reduce disparities, and ultimately provide more equitable and effective care for women undergoing cardiac surgery.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Tricuspid Valve Surgery Outcomes in Women. J Thorac Cardiovasc Surg. 2017;154:202-10.
- [Google Scholar]
- Surgical Outcomes in Women with Marfan Syndrome. J Thorac Cardiovasc Surg. 2014;148:2432-8.
- [Google Scholar]
- Surgical Outcomes of Bicuspid Aortic Valve in Women. J Am Coll Cardiol. 2011;58:1362-70.
- [Google Scholar]
- CABG vs. Medical Therapy in Women with Ischemic Cardiomyopathy. JAMA. 2011;306:751-9.
- [Google Scholar]
- VAD Implantation Outcomes in Women. N Engl J Med. 2009;361:2203-11.
- [CrossRef] [PubMed] [Google Scholar]
- Heart Transplantation vs. LVAD in Women. J Heart Lung Transplant. 2013;32:1170-6.
- [CrossRef] [PubMed] [Google Scholar]







