Translate this page into:
Cardiac PET-CT: A Brief Review of Indications and Feasibility in the Indian Scenario
V. L. Gowthami Rayaprolu Department of Cardiology, Nizam Institute of Medical Sciences (NIMS) Hyderabad, Telangana 500082 India gowthamirao@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Cardiac positron emission tomography (PET) is a functional imaging modality with the predominant indications being an assessment of myocardial perfusion and viability using short-lived positron emitters. PET procedures are used for perfusion assessment only when single-photon emission computed tomography is equivocal. Perfusion agents are ultra short-lived and have limited availability in our country, that is, only at centers with onsite cyclotron. Viability assessment with fluorodeoxyglucose (FDG) is widely performed in many centers across the country due to the availability of FDG. The other important indication is in the detection of inflammatory myocarditis, the most common being cardiac sarcoidosis done with special dietary instructions and FDG as a tracer. This indication is widely used for early detection of myocardial inflammation which would be reversible if treated early. It is also used in the assessment of treatment response. Newer tracer 68 Ga Dotapeptide is also used in this application.
Keywords
cardiac PET-CT
Indian scenario
Introduction
Positron emission tomography (PET) is a functional tomographic imaging modalities in nuclear medicine. It is defined as molecular imaging using short-lived positron emitting radionuclides tagged to organic molecules in order to detect the pathophysiological abnormalities at the cellular level in vivo.
PET has been used for decades as an essential tool to noninvasively image myocardial blood flow and metabolism with higher sensitivity, higher resolution, and quantitative ability. Due to the very short half-life of each of the PET-magnetic particle imaging (MPI) tracers, rest/stress PET-MPI is associated with a very low radiation dose of approximately 2 to 3 mSv (Table 1).
|
Isotope |
Half-life |
Indication |
|---|---|---|
|
Abbreviation: PET, positron emission tomography. |
||
|
15 O-Oxygen |
2 minutes |
Perfusion |
|
13 N-Ammonia |
10 minutes |
Perfusion |
|
82 Rubidium |
76 seconds |
Perfusion |
|
18 F Flurpiridaz |
110 minutes |
Perfusion |
|
18 F-FDG |
109 minutes |
Metabolism and inflammation |
|
68 Ga DOTATATE |
68 minutes |
Inflammation |
However, single photon emission computed tomography (SPECT) is the most commonly used imaging technique due to its availability and low cost.
The use of cyclotron-produced short-lived PET perfusion agents like 13 N-Ammonia and 150 water is restricted only to the sites possessing onsite cyclotron.
This is the major drawback as there are not many cyclotrons in India to support the use of perfusion tracers, and, to date, prohibitively expensive rubidium generator cost makes it a nonviable option in our country, although many universities across the globe with dedicated cardiac units and no cyclotron facility have been using it for the past decade. With all these logistics and economic constraints, SPECT MPI is still the preferred imaging for myocardial perfusion assessment.
Advances in medical imaging technology led to the invention of PET-CT, a hybrid system that combines PET with CT, which is now routinely found in all nuclear medicine departments. As noted above, with such systems, nuclear MPI is routinely coupled with coronary artery calcium (CAC) scanning, allowing assessment and management of coronary atherosclerosis that might not be detected by ischemia testing alone. Coupling of MPI and cardiac computed tomography angiography (CCTA) in the same setting with these systems has also been described.1 Several studies have evaluated hybrid PET-MPI/CCTA with respect to prediction of hemodynamically significant stenosis, as defined by invasive angiography in combination with fraction flow reserve (FFR),2 3 and have demonstrated higher accuracy of the combination than with either modality alone.
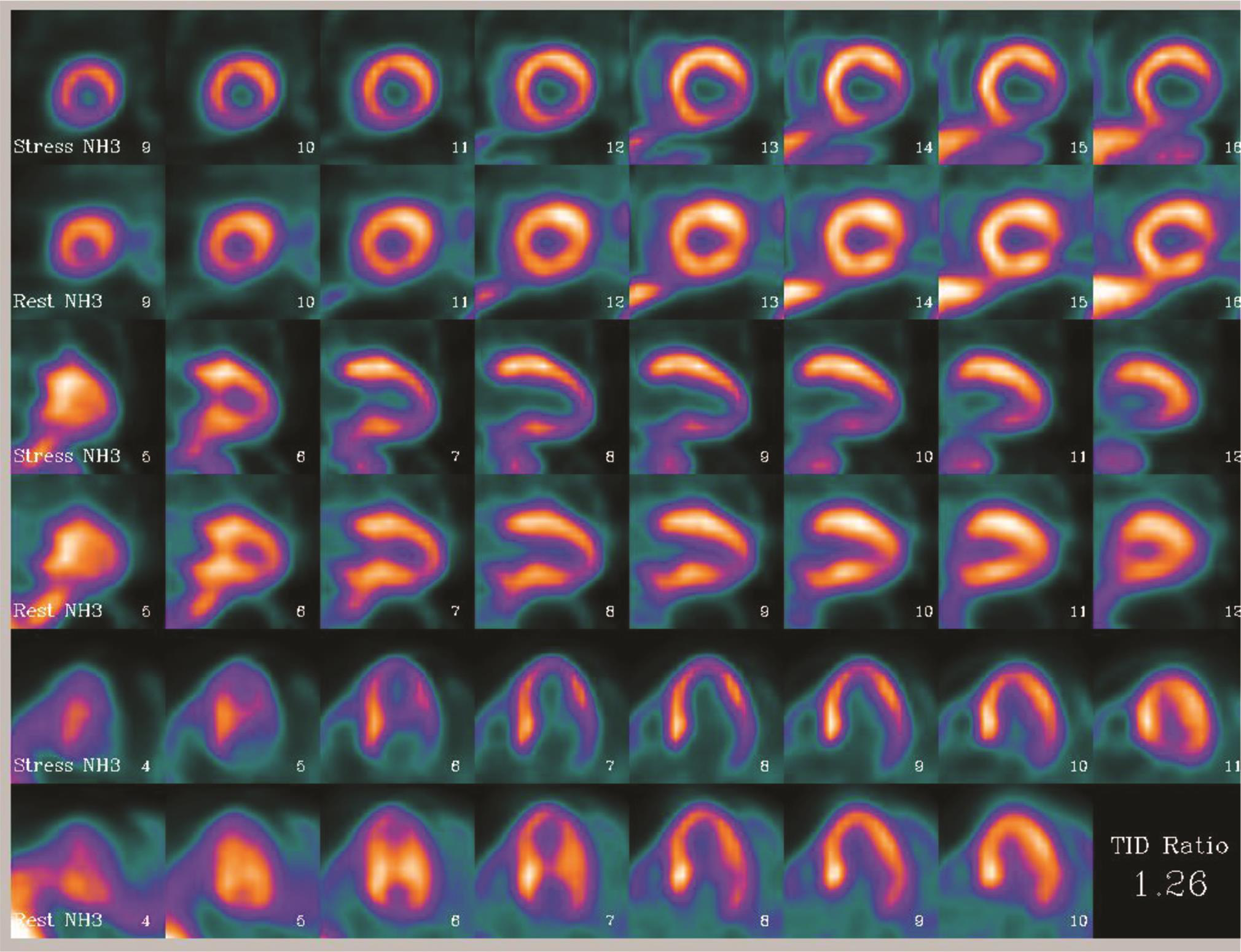
PET-CT is widely used in oncology as it has become a mandate in the majority of solid organ cancers for staging, restaging and treatment monitoring. Hence, many hospitals are equipped with PET-CT scanners, which are also available for cardiac applications. The systems with 64 or 128 slice CT would be able to perform calcium scoring, CT coronary angiogram (CAG), and, if necessary, functional information at one go (Fig. 1).
-
Fig. 1 13N-ammonia stress PET images showing perfusion defects in apico inferior and lateral wall segments, which are showing filling in rest images suggestive of inducible ischemia in LAD and LCX territories. Abbreviations: LAD, left anterior descending; LCX, left circumflex; PET, positron emission tomography.
Fig. 1 13N-ammonia stress PET images showing perfusion defects in apico inferior and lateral wall segments, which are showing filling in rest images suggestive of inducible ischemia in LAD and LCX territories. Abbreviations: LAD, left anterior descending; LCX, left circumflex; PET, positron emission tomography.
Hybrid PET-MRI systems are appearing in a few research and institutional sites globally and also in India. These systems provide both functional and anatomical information simultaneously. One synergistic effect is the ability of the MRI to distinguish the subepicardial from the subendocardial flow.
18F is a preferred positron emitter in PET imaging with its relatively long half-life and flexible chemistry to get labeled with various ligands. 18F-Flurodeoxyglucose (FDG) is the workhorse in all PET-CT scanner facilities across the globe not only for oncological and neurological applications but also for cardiac pathologies. It is used for myocardial viability and myocardial inflammation assessment.
While novel 18F-labeled perfusion radiotracers are being developed, F-18 flurpiridaz is the most prominent one, as these radiotracers are still evaluated in clinical phase 3 trials which may make PET MPI with absolute flow quantification a more widely available method. 18F-fluoromisonidazole (FMISO) is another most commonly used PET tracer for measuring hypoxia. Retention of 18F-FMISO correlates with the severity of hypoxia.4
Applications of Cardiac PET-CT
Myocardial Perfusion Imaging
PET perfusion tracers are a gold standard for measuring blood flow in the myocardium.5 Tracers with high-extraction fraction and myocyte retention qualify them to be used for assessment of myocardial perfusion in the diagnosis and evaluation of coronary artery disease (CAD). Absolute quantitative assessment of myocardial blood flow and coronary flow reserve with perfusion tracers 82Rb, 15O-water, and 13N-Ammonia are well-established and have appropriate dosimetry and safety profile; however, they are only conducted in centers with onsite cyclotron and rubidium generators in India.
Stress and rest myocardial perfusion imaging is performed for detection or demonstration of inducible ischemia on the same day (Fig. 2) as these tracers are short-lived. When exercise-induced stress is not feasible because the length of the test exceeds the radiotracer half-life or there are patients who cannot exercise, pharmacological stress is induced by administering dipyridamole, adenosine, regadenoson, or dobutamine when the patient is ready to be imaged.6 7 Indications for MPI are the same as CT CAG or SPECT,8 apart from an additional few differences.

-
Fig. 2 Indications for stress myocardial perfusion imaging.
Fig. 2 Indications for stress myocardial perfusion imaging.
PET scan is performed in place of, but not in addition to SPECT, except when SPECT findings are inconclusive or discordant with patient's other clinical data.9
The advantages of PET over SPECT are high-system resolution, better attenuation correction with PET CT, and high-energy photons, which would overcome the attenuation artifacts, resulting in higher sensitivity (Figs. 3 4).

-
Fig. 3 (A) SPECT myocardial perfusion VLA images showing diffuse hypoperfusion in the inferior wall. (B) 13N-ammonia PET scan images showing normal uptake in inferior wall, thus confirming the attenuation artifact. Abbreviations: PET, positron emission tomography; SPECT, single photon emission computed tomography; VLA, very large array.
Fig. 3 (A) SPECT myocardial perfusion VLA images showing diffuse hypoperfusion in the inferior wall. (B) 13N-ammonia PET scan images showing normal uptake in inferior wall, thus confirming the attenuation artifact. Abbreviations: PET, positron emission tomography; SPECT, single photon emission computed tomography; VLA, very large array.

-
Fig. 4 (A) MDCT image showing high-calcium score. (B) Stress 13N-ammonia short axis perfusion slice showing normal perfusion in the entire myocardium, thus obviating the need for any further intervention for the asymptomatic patient with high-calcium score. Abbreviation: MDCT, multiple detector computed tomography.
Fig. 4 (A) MDCT image showing high-calcium score. (B) Stress 13N-ammonia short axis perfusion slice showing normal perfusion in the entire myocardium, thus obviating the need for any further intervention for the asymptomatic patient with high-calcium score. Abbreviation: MDCT, multiple detector computed tomography.
Absolute quantitation of myocardial blood flow (MBF) by PET plays a significant role in the clinical evaluation of epicardial and microvascular CAD.10 Apart from onsite cyclotron and the expensive 82 Rb generator, there is need for specific hardware and software in the scanner for execution and setting of reference values, which restricts its availability in our country to just less than a handful of institutes.
82Rb perfusion scans also are used in estimation of coronary flow reserve in heart transplantation patients which would be of help in prognostication.11
Myocardial Viability
FDG is used to detect myocardial metabolism. It is taken up by the cardiomyocyte by glucose transporter(GLUT) receptors and enters the glucose metabolism, wherein it is acted upon by hexokinase and gets converted to FDG6 phosphate.12 Beyond this, it would not enter further, as there are no enzymes in the cell to act upon.
FDG imaging for viability is usually performed using glucose load and IV insulin to improve the FDG uptake. Viable cells show FDG uptake due to a shift to preferential glucose metabolism rather than fatty acid. The comparison between myocardial segmental perfusion and metabolism provides information regarding the amount of normal and nonviable myocardium.
In CAD patients with contractile dysfunction to differentiate infarct from stunning or hibernation in cases of acute ischemia, and demonstration of viable myocardium in chronic total occlusions, are the major indications for viability scan with 18F-FDG. This plays a very important role in selecting late presenting acute myocardial infarction and ischemic cardiomyopathy patients for intervention or medical management, which would impact outcome.
Viability scan is done in two steps—the first step is rest perfusion scan either on SPECT or with PET perfusion tracers, which would provide a roadmap (Fig. 4) to follow and determine whether there is further need for metabolism assessment with FDG. A perfusion defect persistent in the stress study would confirm infarct or nonviable tissue, whereas the defect showing FDG uptake would be indicative of viable myocardium, which is salvageable (Figs. 5 6). The degree to which left ventricular (LV) function recovers after revascularization depends on the amount of “viable myocardium.” To achieve at least a 5% increase in left ventricular ejection fraction (LVEF) requires the presence of “viability” in approximately 15 to 25% of the LV.13

-
Fig. 5 Rest ammonia perfusion slices displayed on top row, and FDG metabolism in lower row shows matching defects in both perfusion and metabolism, qualifying the defect as infarct with nonviable tissue. Abbreviation: FDG, fluorodeoxyglucose.
Fig. 5 Rest ammonia perfusion slices displayed on top row, and FDG metabolism in lower row shows matching defects in both perfusion and metabolism, qualifying the defect as infarct with nonviable tissue. Abbreviation: FDG, fluorodeoxyglucose.

-
Fig. 6 Top row FDG images and bottom row perfusion images. Perfusion defect is seen in the inferior wall on the short axis and VLA images show FDG concentration–perfusion metabolism mismatch suggests salvageable viable tissue. Abbreviations: FDG, fluorodeoxyglucose; VLA, very large array.
Fig. 6 Top row FDG images and bottom row perfusion images. Perfusion defect is seen in the inferior wall on the short axis and VLA images show FDG concentration–perfusion metabolism mismatch suggests salvageable viable tissue. Abbreviations: FDG, fluorodeoxyglucose; VLA, very large array.
Myocardial Inflammation/Myocarditis
Increased glucose metabolism is a hallmark of inflammation and can be visualized effectively using 18F-FDG. Under aerobic conditions, cardiomyocyte is an omnivore and utilizes free fatty acids, glucose and, to a lesser extent, amino acids. FDG uptake in myocardium under fasting is also variable, which might cause false positives.
This shows the need for better protocols to suppress myocyte glucose uptake for a PET-based diagnostic workup of inflammatory imaging, particularly in cardiac sarcoidosis and other myocarditis of various causes like autoimmune, bacterial, viral, etc.
The most commonly used current protocols for myocardial suppression include a very high-fat, low-carbohydrate, protein preferred diet and a heparin load before imaging.14 A perfusion and metabolism mismatch is a more specific finding suggestive of inflammation, followed by focal areas’ FDG uptake with no perfusion defect (Fig. 7). Perfusion defect with no FDG uptake suggests scarring, which suggests irreversible muscle damage and scarring with poor prognosis.

-
Fig. 7 (A) SPECT perfusion images in a patient with suspected cardiac sarcoidosis and normal coronaries, showing perfusion defects in the septum and inferior walls. (B) Suppressed FDG images show uptake corresponding to the perfusion defects, that is, in the septum and inferior wall. (C, D, E) FDG body survey showed metabolically active hilar nodes and splenic lesion TES guided biopsy of hilar nodes showed noncaseating granulomas and confirmed the diagnosis of cardiac sarcoidosis. Abbreviations: FDG, fluorodeoxyglucose; SPECT, single photon emission computed tomography.
Fig. 7 (A) SPECT perfusion images in a patient with suspected cardiac sarcoidosis and normal coronaries, showing perfusion defects in the septum and inferior walls. (B) Suppressed FDG images show uptake corresponding to the perfusion defects, that is, in the septum and inferior wall. (C, D, E) FDG body survey showed metabolically active hilar nodes and splenic lesion TES guided biopsy of hilar nodes showed noncaseating granulomas and confirmed the diagnosis of cardiac sarcoidosis. Abbreviations: FDG, fluorodeoxyglucose; SPECT, single photon emission computed tomography.
FDG PET aids in early detection of inflammation and monitors the treatment response in cases of cardiac sarcoid (Fig. 8), with high-sensitivity and specificity comparable to other imaging modalities. It offers whole body imaging, providing information regarding the multifocal disease, which also helps in guiding the intervention like targeted biopsies from more amenable sites. Semiquantitative indices of the total 18F-FDG uptake such as cardiac metabolic volume and cardiac metabolic activity similarly contain predictive information and appear to be useful for estimating treatment responses.15

-
Fig. 8 (A) FDG scan shows mediastinal uptake nodal uptake and diffuse myocardial uptake in an enlarged heart which is treated as inflammatory cardiomyopathy. (B) Posttreatment scan—absent nodal uptake and myocardial uptake with a decrease in size of heart—is indicative of good response. Abbreviation: FDG, fluorodeoxyglucose.
Fig. 8 (A) FDG scan shows mediastinal uptake nodal uptake and diffuse myocardial uptake in an enlarged heart which is treated as inflammatory cardiomyopathy. (B) Posttreatment scan—absent nodal uptake and myocardial uptake with a decrease in size of heart—is indicative of good response. Abbreviation: FDG, fluorodeoxyglucose.
Infective Endocarditis
Vegetations and abscesses of native and prosthetic valves can be visualized with 18F-FDG PET/CT, although with a lower and clinically insufficient sensitivity (~40%) and a specificity of approximately 70 to 100%.16 Other investigators have confirmed the high-sensitivity and specificity of 18F-FDG PET/CT for the detection of septic emboli and metastatic infections in patients with definite infectious endocarditis according to the Duke criteria.17
Vasculitis
Vascular imaging with 18F-FDG PET/CT may prove useful for establishing the diagnosis of vasculitis, especially in patients with nonspecific symptoms. Furthermore, it delineates the spread of active disease throughout the great vessels (H pg641). The intensity of vascular 18F-FDG uptake serves as a measure of the degree of inflammation and of its response to therapy, and, as suggested by one investigation, reflects the treatment response more accurately than contrast-enhanced MRI.18
Emerging Trends in PET
Active Mineral Deposition and Calcification of Atherosclerotic Plaques
18F sodium fluoride (18F-NaF) has recently emerged as another tool for probing the pathophysiology of atherosclerosis. The findings reported in both large arterial vessels and coronary vessels studies imply that 18F-FDG and 18F-NaF target atherosclerotic plaques but different aspects and, probably, different phases of dynamic plaque biology. Lesional 18F-FDG uptake likely precedes uptake of 18F-NaF as an indicator of active calcification. Vascular uptake of either radiotracer may reflect potential plaque instability—one as a consequence of high-inflammation and the other as a consequence of plaque rupture and active mineral deposition.19
68 Ga DOTATATE is a somatostatin receptor imaging agent which would be an alternative to FDG in the detection of myocardial inflammation. They also concentrate on the activated macrophages, which overexpress SSTR type 2 receptors, thus showing uptake in inflammatory sites. 68Ga-DOTANOC PET/CT can be used as an adjunct imaging modality in patients with suspected cardiac sarcoidosis (CS), preferably as an imaging substitute for the obsolete 67Ga citrate scintigraphy. In a small cohort of patients with suspected CS, cardiac Ga-DOTANOC PET/CT had excellent diagnostic accuracy and had the advantage over 18F-FDG PET/CT in that no prescan fasts, diets, or infusions were required.20 This tracer has fast blood clearance and is not only superior to FDG in identifying vulnerable plaque21 but also shows greater specificity as an inflammation imaging target.22
Conclusion
Cardiac imaging with PET-CT offers highly sensitive myocardial perfusion imaging; however, with limited availability of tracers, it restricts the use to only the centers with onsite cyclotron. On the other hand, myocardial viability evaluation with FDG is the preferred cardiology indication in almost all PET centers across the country as well as globally. PET-CT in inflammatory cardiomyopathies with FDA also took off in recent years, providing very useful information regarding the myocardial involvement, especially in cardiac sarcoidosis, avoiding the invasive endomyocardial biopsies. 68Ga DOTATATE is making its presence in cardiac inflammation imaging with encouraging results. However, further studies are required for it to replace FDG; also, its availability only in centers with Germanium-Ga generator is a limitation. Although many other new PET tracers are coming to light off late, here we intend to highlight those which are used in the Indian context.
Conflict of Interest
None declared.
References
- Diagnosing coronary artery disease with hybrid PET/CT: it takes two to tango. J Nucl Cardiol. 2013;20(05):874-890.
- [Google Scholar]
- Cardiac positron emission tomography/computed tomography imaging accurately detects anatomically and functionally significant coronary artery disease. Circulation. 2010;122(06):603-613.
- [Google Scholar]
- Hybrid imaging using quantitative H215O PET and CT-based coronary angiography for the detection of coronary artery disease. J Nucl Med. 2013;54(01):55-63.
- [Google Scholar]
- Development of F-18-labeled fluoroerythronitroimidazole as a PET agent for imaging tumor hypoxia. Radiology. 1995;194(03):795-800.
- [Google Scholar]
- Searching for novel PET radiotracers: imaging cardiac perfusion, metabolism and inflammation. Am J Nucl Med Mol Imaging. 2018;8(03):200-227.
- [Google Scholar]
- Burger C, von Schulthess GK, Kaufmann PA. Bicycle exercise stress in PET for assessment of coronary flow reserve: repeatability and comparison with adenosine stress. J Nucl Med. 2003;44(02):146-154.
- [Google Scholar]
- Current methods of pharmacologic stress testing and the potential advantages of new agents. J Nucl Med Technol. 2009;37(01):14-25.
- [Google Scholar]
- Dorbala S, Di Carli MF, Delbeke D, et al. SNMMI/ASNC/SCCT Guideline for cardiac SPECT/CT and PET/CT 1.0. Available at http://www.snmmi.org/guidelines. Accessed April 22, 2020
- SNMMI/ASNC/SCCT guideline for cardiac SPECT/CT and PET/CT 1.0. J Nucl Med. 2013;54(08):1485-1507.
- [Google Scholar]
- Cardiac PET imaging for the detection and monitoring of coronary artery disease and microvascular health. JACC Cardiovasc Imaging. 2010;3(06):623-640.
- [Google Scholar]
- Serial assessment of coronary flow reserve by Rb-82 PET predicts mortality in heart transplant recipients. JACC Cardiovasc Imaging. 2020;13:109-120. (1 Pt 1)
- [Google Scholar]
- Multimodality imaging in the assessment of myocardial viability. Heart Fail Rev. 2011;16(04):381-395.
- [Google Scholar]
- Improvement of left ventricular ejection fraction, heart failure symptoms and prognosis after revascularization in patients with chronic coronary artery disease and viable myocardium detected by dobutamine stress echocardiography. J Am Coll Cardiol. 1999;34(01):163-169.
- [Google Scholar]
- Incidence of abnormal positron emission tomography in patients with unexplained cardiomyopathy and ventricular arrhythmias: The potential role of occult inflammation in arrhythmogenesis. Heart Rhythm. 2015;12(12):2488-2498.
- [Google Scholar]
- Positron emission tomography/computed tomography for diagnosis of prosthetic valve endocarditis: increased valvular 18F-fluorodeoxyglucose uptake as a novel major criterion. J Am Coll Cardiol. 2013;61(23):2374-2382.
- [Google Scholar]
- (18)F-FDG PET/CT for early detection of embolism and metastatic infection in patients with infective endocarditis. Eur J Nucl Med Mol Imaging. 2010;37(06):1189-1197.
- [Google Scholar]
- Value of F-18 FDG hybrid camera PET and MRI in early Takayasu aortitis. Eur Radiol. 2003;13(02):400-405.
- [Google Scholar]
- Early aortic valve inflammation precedes calcification: a longitudinal FDG-PET/CT study. Atherosclerosis. 2015;238(02):165-172.
- [Google Scholar]
- A dual tracer (68)Ga-DOTANOC PET/CT and (18)F-FDG PET/CT pilot study for detection of cardiac sarcoidosis. EJNMMI Res. 2016;6(01):52.
- [Google Scholar]
- 68Ga-DOTATATE PET/CT for the detection of inflammation of large arteries: correlation with18F-FDG, calcium burden and risk factors. EJNMMI Res. 2012;2(01):52.
- [Google Scholar]







