Translate this page into:
Birth Weight, Current Weight, and Weight Dynamism from Birth to Adulthood as Measure of Outcome in Heart Failure
*Corresponding author: Sadanand T. Indi, Department of Cardiology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India. mr.sadanand.indi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: I Sadanand. Birth Weight, Current Weight, and Weight Dynamism from Birth to Adulthood as Measure of Outcome in Heart Failure. Indian J Cardiovasc Dis Women. 2025;10:41-4. doi: 10.25259/IJCDW_23_2024
Abstract
Objectives:
Among the non-communicable disease, the cardiovascular disease is the major cause of mortality worldwide. The risk factors include hypertension, diabetes mellitus increasing age and gender, and dyslipidemia. Recently, much attention has been paid to the impact of weight in determining the cardiovascular events and it’s role in development of chronic disease. Studies have been published for fetal origin for adult disease; one among them is barker’s hypothesis. Furthermore, epidemiological study proposes decremental effects of birth weight outside the normal range. Our study focuses on significance of birth weight, weight dynamism from birth to adulthood for correlation with heart failure (HF) in adults.
Materials and Methods:
Imaging studies were done with echocardiography (ECHO) of 2.5–3.5 Mhz transducers. Patients were grouped as Group A and B. Group A is asymptomatic, healthy population. Group B patients have failure signs and symptoms. Both group undergone to 2D ECHO, necessary tests, and body mass index measured.
Results:
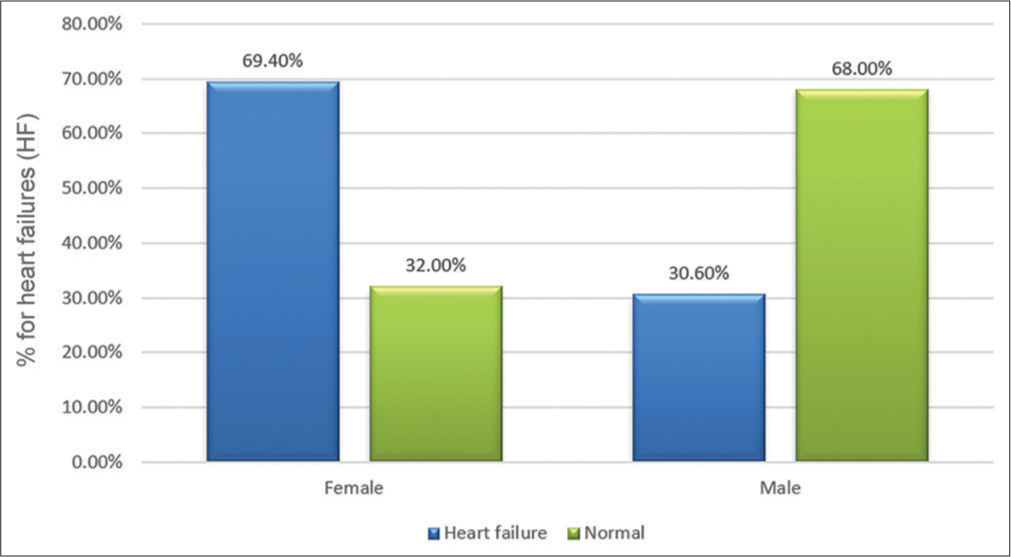
In our study, we collected data from 100 subjects. Out of 50 patients in case, group age of patient ranges from 50 to 60 years. Among the control group, age of patients ranges from 50 to 60 years. Mean age of patient in case group is 58.4 ± 3.36 year. Mean age of patients in Group A is 56.6 ± 3.02 years. Birth weight among the patients with HF ranges from 1.5 to 3.5 kg. Total number of patients having low birth weight (LBW) is 44 among case group. None of the patients were having LBW in the control group and it was statistically significant (P < 0.001). Thus indicating, there is a higher incidence of HF in patients having LBW. Mean birth weight among patients with HF was 2.14 ± 0.267 kg and among control group was 3.01 ± 0.276 kg. Incidence of HF was more among women than men group.
Conclusion:
The LBW associated HF and has an inverse relationship with cardiovascular function; also, adult obese population have an increased risk of HF. Similarly, severe left ventricular dysfunction had high present weight and women had high risk of HF compared to men group.
Keywords
Birth weight
Low and high birth weight
Obesity
ABSTRACT IMAGE
INTRODUCTION
Cardiovascular disease (CVD) is among the leading causes of mortality overall, and risk factors include age, gender, lipid levels, smoking, hypertension, and diabetes; these risk factors are reasons for 75–80% of individuals to develop CVD.[1] Recent studies focus more on early life exposures such as fetal environment, birth weight, and development of chronic adult diseases. The “Barker hypothesis,” which suggests fetal origins of adult disease, has been tested by various epidemiological studies that describe the detrimental effects of birth weight that is out of normal value.[2] Specifically, low birth weight (LBW), defined as <6 lbs, is associated with an increased risk of chronic adult conditions persistently, especially CVD, diabetes, and metabolic syndrome. Data on the role of birth weight in predicting heart disease is limited. In addition, the prevalence of maternal obesity has increased, and it has led to a heightened large for gestational age infants, representing another group at risk for adverse adult health outcomes due to the intrauterine environment.[3] This present study aims to evaluate the significance of birth weight and weight changes from birth to adulthood in heart failure (HF) in adults.
MATERIALS AND METHODS
We studied at Nizam’s Institute of Medical Sciences hospital from June 2022 to October 2022. Patients from the Cardiology and General Medicine Outpatient Departments were enrolled in the study. One hundred patients were included based on the inclusion and exclusion criteria. The study received approval from the NIMS Ethics Committee. Informed written consent was obtained before the study began. Initial investigations and vitals, including N-terminal-Pro Brain Natriuretic Peptide (NT-pro BNP) levels, were performed during the visit. Simultaneously, the patient’s weight and height were measured.
All echocardiography (ECHO) examinations were performed using a handheld probe with 2.5–3.5 MHz transducers. ECHO was performed according to protocol using M-mode, color Doppler ECHO. The corresponding views and documented findings assessed the left ventricular ejection fraction (LVEF) and diastolic dysfunction. Patients included were classified into Groups A and B: Group A had no cardiac symptoms and were not in HF, while Group B consisted of symptomatic patients. Both groups underwent 2D ECHO, necessary tests, and body mass index (BMI) measurements.
Statistical analysis
Mean and standard deviation were used to analyze the continuous variable; similarly, Pearson’s Chi-square test was used for categorical variables, and a t-test was applied for continuous variables. All data were evaluated at the end of the study, and statistical significance was determined with P < 005. The receiver operating characteristic curve determined the cutoff age.
RESULTS
In our study, we collected data from 100 subjects. Fifty patients were either newly diagnosed with HF or were known cases of HF on medication. Fifty individuals were randomly selected from the general population without HF, attending routine health checkups, non-cardiac surgical procedures, or other ailments at the cardiology or general medicine outpatient departments. All patients were screened with 2D ECHO to assess left ventricular function, and their birth weights were collected.
Among the 50 patients in the case group, cases had ages between 50 and 60 years. In the control group, the age range was also 50–60 years. The case group patients had a mean age of 58.4 ± 3.36 years, while the control group had a mean age of 56.6 ± 3.02 years. The birth weight among patients with HF ranged from 2.9 kg with a standard deviation of 0.222. A total of 44 patients in the case group had LBW, while none in the control group had LBW, which was statistically significant (P<0.001). This suggests a higher incidence of HF in patients with LBW. The mean birth weight among patients with HF was 2.14 ± 0.267 kg, compared with 3.01 ± 0.276 kg in the opposite group.
The incidence of HF was higher among women than men. Among patients with HF, 19 were overweight, and 31 were obese, while among the controls, 42 had a normal BMI, eight were overweight, and none were obese. The mean BMI in the HF group was 30.61 ± 1.6 kg/m2. The mean present weight was 63.91 kg with a standard deviation of 8.91 kg, and the mean age in the control group was 58.9 years. The mean LVEF in patients with HF was 28.58%, while in the control group, it was 59.44%. The mean NT-pro BNP level in the case group was 25,507.36, compared to 215 in the control group.
DISCUSSION
The study shows the inverse correlation between birth weight and HF risk. Furthermore, there is enough evidence available that this association persists after accounting for BMI in childhood and adolescence [Table 1]. Findings include the development of early HF among females who have LBW and subsequently gain weight in young adulthood. This group is affected by HF as early as 50, around 5–8 years younger, compared to the reference group [Figure 1]. In addition, the inverse association between birth weight and the risk of HF is seen, even with the birth weight in the 1.5–3.5 kg range, indicating that extremely LBWs do not solely drive this association.
| BMI | Group | Total | |
|---|---|---|---|
| Cases | Controls | ||
| Normal | 0 | 42 | 42 |
| Overweight | 19 | 8 | 27 |
| Obese | 31 | 0 | 31 |
| Total | 50 | 50 | 100 |
| P<0.001 | |||
BMI: Body mass index
- Excess risk of developing early heart failure women with low birth weight.
Among the various variables, childhood BMI showed the least possible association with the development of cardiac symptoms related to HF. The other studies, which included neonatal weight, childhood overweight, and adolescent overweight, did not significantly have the risk of cardiac disease. However, considering the birth weight and increase in BMI, adolescent weight gain no longer showed a significant risk of coronary heart disease (CHD).
The various observational studies show an association between LBW[1,4,5] and CHD without considering the BMI in developmental adolescents and adults. A few studies have examined the combined association of birth weight and young adult BMI with the risk of HF. A survey by Wang et al., observed an additive interaction between decreasing birth weight and overweight/obesity, particularly among women, and this persisted independently of lifestyle factors in later life.[6] Similarly, in our study, obesity and overweight emerged as significant risk factors for HF [Figure 2].
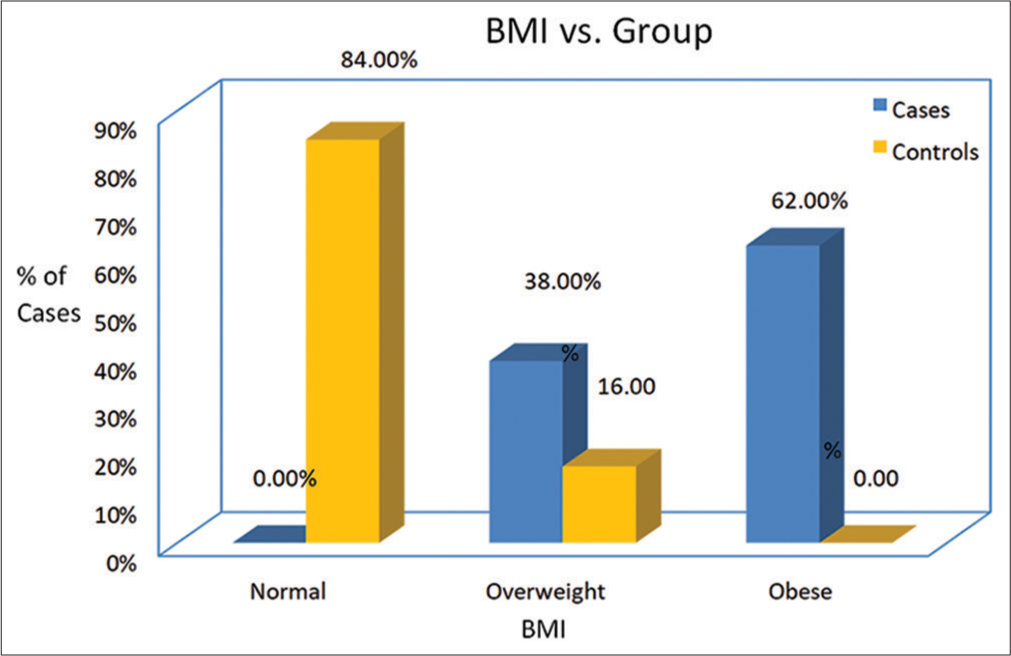
- Comparison of body mass index in cases and control group. (BMI: Body mass index).
The study conducted by Smith et al., showed that birth weight is an independent risk factor for CVD.[7] Similarly, a cohort study by Sukuki et al., suggested that unfavorable fetal environmental factors implicated in LBW may bring permanent changes in organ development and metabolism that are important in the development of hypertension, lipid disorders, and adult-onset diseases.[8] Our study also proposes that the future risk of HF is the result of LBW, adolescent overweight, and current weight interaction.
A study by Tian et al., demonstrated a robust inverse relationship between HF and birth weight. Similarly, our study confirmed that LBW and HF are inversely related.[9] LBW and adult-onset overweight are detrimental risk factors for the early development of HF, and our findings suggest adolescent-onset weight gain is an important risk factor for early HF development.
This well-powered study is based on reliable data from the patient population on various important factors. The study also benefited from a low mortality rate before age 20. It is register-based details on HF outcomes, with complete follow-up of patients. Although there are reliable data on birth weight, information on gestational age and maternal factors is unavailable.
CONCLUSION
Increased risk of HF is seen more with LBW and has an inverse relationship with cardiovascular function. In addition, obese adults are at a heightened risk of HF. Similarly, higher current weight is associated with deranged left ventricular dysfunction, and females are at a greater risk of developing HF compared to men.
Ethical approval
The research/study was approved by the Institutional Review Board at Nizam’s Institute of Medical Sciences, number EC/NIMS/3030/2020, dated September 26, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship: Nil.
References
- The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. J Am Coll Cardiol. 2022;80:2361-71.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of the Intrauterine Environment on Childhood Growth. Br Med Bull. 1997;53:81-95.
- [CrossRef] [PubMed] [Google Scholar]
- Birth Weight is Inversely Associated with Incident Coronary Heart Disease and Stroke among Individuals Born in the 1950s: Findings from the Aberdeen Children of the 1950s Prospective Cohort Study. Circulation. 2005;112:1414-8.
- [CrossRef] [PubMed] [Google Scholar]
- Longitudinal Study of Birth Weight and Adult Body Mass Index in Predicting Risk of Coronary Heart Disease and Stroke in Women. BMJ. 2005;330:1115.
- [CrossRef] [PubMed] [Google Scholar]
- Associations of Birth Weight and Later Life Lifestyle Factors with the Risk of Cardiovascular Disease in the USA: A Prospective Cohort Study. eClinicalMedicine. 2022;51:101570.
- [CrossRef] [PubMed] [Google Scholar]
- The Impact of Birth Weight on Cardiovascular Disease Risk in the Women's Health Initiative. Nutr Metab Cardiovasc Dis. 2016;26:239-45.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between Birth Weight and Cardiovascular Risk Factors in Japanese Young Adults. Am J Hypertens. 2000;13:907-13.
- [CrossRef] [PubMed] [Google Scholar]
- Contribution of Birth Weight and Adult Waist Circumference to Cardiovascular Disease Risk in a Longitudinal Study. Sci Rep. 2017;7:9768.
- [CrossRef] [PubMed] [Google Scholar]







