Translate this page into:
Bedside Lung Ultrasound in Patients with Acute Decompensated Heart Failure—An Observational Study
Srikiran Jakkula, MD, DM Department of Cardiology, Nizam's Institute of Medical Sciences Punjagutta, Telangana 500082 India srikiran.jakkula@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract

This study was done to evaluate the lung ultrasound findings such as Kerley A and Kerley B lines and the correlation between them with duration of hospital stay, where patients with Kerley A lines had longer duration of hospital stay even though it was statistically insignificant. N-terminal pro-brain natriuretic peptide levels were higher in female patients when compared with males in acute decompensated heart failure.
Keywords
decompensated heart failure
ultrasound
Introduction
Dyspnea is one of the most common presenting problems in the emergency department and one of the common causes of hospitalization in the intensive care unit. The initial evaluation that is based on history, clinical examination, electrocardiography, X-ray chest, and BNP or NT pro-BNP (N-terminal pro-brain natriuretic peptide) levels is important in the dyspnea evaluation.1 Over the past 20 years, lung ultrasound (LUS) has become an essential part in the evaluation of acute onset shortness of breath, demarcating between acute decompensated heart failure, and other noncardiac causes of dyspnea, mostly the acute exacerbation of chronic obstructive pulmonary disease (COPD).1 LUS also has many advantages over classical evaluation. It is a quick, easily available noninvasive tool done at bedside by clinicians with portable machine.1 The standard of care has been improved by LUS in the diagnosis and monitoring of acute decompensated heart failure, and it should be used in routine practice to incorporate clinical examination and common investigations.1
In the past years, LUS has gained wider applications.1 While performing the LUS, pleural line is visible just beneath the soft tissue of the chest wall. Under normal circumstances, the layers of pleura move upon each other; this hyperechoic line makes a horizontal “sliding” movement, which is synchronous with respiratory movements. A homogenous “foggy-like” image interrupted by several horizontal reverberations of the pleural line is divided by a fixed period (Kerley A lines). The vertical reverberations called Kerley B lines appear when the volume of air in the lungs decreases due to interstitial accumulation, deposition of blood or collagen. The objective of the study is to evaluate the bedside LUS findings in patients with acute decompensated heart failure.
Materials and Methods
This study was done in a tertiary care center as an observational cross-sectional study with a study period of 3 months, from July 2021 to September 2021. The study population included all the patients admitted to intensive coronary care unit (ICCU) with acute decompensated heart failure. Patients with age over 18 years were included in the study. Exclusion criteria included patients with age less than 18 years, patients with prior history of lung disorders such as COPD, interstitial lung diseases, bronchiectasis, and pneumothorax, and patients with post cardiopulmonary resuscitation.
All patients satisfying inclusion and exclusion criteria were taken into study. Bedside LUS was performed and findings were recorded. The study was done in ICCU, Nizam's Institute of Medical Sciences, on random day during patient's hospital stay. The LUS findings primarily focused on Kerley A and Kerley B lines that were correlated with hospital stay duration and statistical analysis was performed using mean and standard deviation. Analysis was also done between sex of the patient and the levels of NT pro-BNP.
Statistical Analysis
Statistical analysis was done in MS Excel 2021. Results on continuous variables will be presented as mean and standard deviation. t-test will be used for statistical analysis. p < 0.05 will be considered as statistically significant.
Results
Demographic Profile
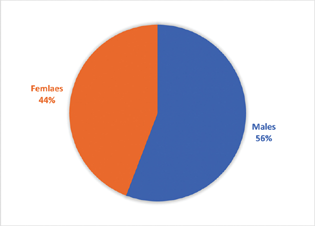
The average age of presentation in males and females were 58.5 and 60 years, respectively. Out of 43 patients with acute decompensated heart failure, 24 were males (56%) and 19 were females (44%), as shown in Fig. 1.
-
Fig. 1 Pie diagram showing distribution of cases according to sex.
Fig. 1 Pie diagram showing distribution of cases according to sex.
LUS findings for Kerley A and Kerley B lines were recorded on 43 patients with acute decompensated heart failure. The Kerley A and Kerley B lines were correlated with hospital stay duration. Kerley A lines were found in 8 out of 43 patients, which were correlated with the duration of hospital stay (mean: 7.75 days, standard deviation: 3.11 days). Kerley B lines were found in 35 out of 43 patients, which were correlated with the duration of hospital stay (mean: 6.14 days, standard deviation: 2.01 days). p-Value obtained was 0.19 that was statistically insignificant (Table 1). Further analysis was done between sex of the patient and the NT pro-BNP levels. NT pro-BNP values were analyzed from 7 males and females. Males had a mean NT pro-BNP levels of 5,146 and standard deviation of 2,389.9. Females had a mean NT pro-BNP levels of 8,666 and standard deviation of 7,288. Calculated p-value was 0.264 that was statistically insignificant (Table 2).
|
LUS findings (n = 43) |
Duration of hospital stay in days |
p-Value |
|---|---|---|
|
Kerley A lines (n = 8) |
Mean: 7.75 |
0.19 |
|
Standard deviation: 3.11 |
||
|
Kerley B lines (n = 35) |
Mean: 6.14 |
|
|
Standard deviation: 2.01 |
Abbreviation: LUS, lung ultrasound.
|
Sex |
NT pro-BNP levels |
p-Value |
|---|---|---|
|
Males (n = 7) |
Mean: 5,146 |
0.264 |
|
Standard deviation: 2,389.9 |
||
|
Females (n = 7) |
Mean: 8,666 |
|
|
Standard deviation: 7,288 |
Abbreviation: NT pro-BNP, N-terminal pro-brain natriuretic peptide.
Discussion
According to Praveen et al, the mean Kerley B lines were higher among the patients who were admitted for more than 10 days at the time of admission.2 None of the other studies were available to compare these results. Males outnumbered females in this study. About 55.8% (n = 24) patients were males and 44.1% (n = 19) were females. In a study by Miglioranza et al, ∼61% of all the patients with heart failure were males.3 Coiro et al also observed similar results in their study.4 In a study by Prosen et al, ∼73% of the patients with acute heart failure-related dyspnea were males.5 In a study by Platz et al, ∼71% of the patients were males.6 In a study by Mar Domingo et al, 72% of the patients were males.7
In our study, NT pro-BNP levels were higher in females with mean of 8,666 and standard deviation of 7,288, when compared with males with mean of 5,146 and standard deviation of 2,389. Calculated p-value was 0.26 that was statistically insignificant. In a study done by Hack-Lyoung Kim et al, NT pro-BNP levels were significantly higher in patients with events compared with those without, in both genders (p < 0.001 for each).8 A higher NT pro-BNP level was an independent predictor of events (highest vs. lowest tertile: hazard ratio, 1.74; 95% confidence interval, 1.25–2.43; p = 0.001) in men, even after controlling for potential confounders.8 The NT pro-BNP level seems to be a more valuable marker in the prediction of heart failure readmissions and long-term mortality in men than in women.8 LUS is being used commonly in the approach for patients with heart failure because it has proven to have high diagnostic accuracy, nevertheless we must follow a structured and standardized protocol to report the same findings.9 10
Conclusion
This study was done to evaluate the LUS findings such as Kerley A and Kerley B lines and the correlation between them with the duration of hospital stay, where patients with Kerley A lines had longer duration of hospital stay even though it was statistically insignificant. NT pro-BNP levels were higher in female patients when compared with males in acute decompensated heart failure. Bedside LUS was also cost-effective in compared with the NT pro-BNP test.
Limitations of the Study
-
This study was a cross-sectional study and lacked follow-up analysis and evaluation.
-
NT pro-BNP levels were not analyzed in all patients.
Conflict of Interest
None declared.
References
- Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134(01):117-125.
- [Google Scholar]
- Evaluation of lung ultrasound with clinical congestion score in diagnosis and clinical outcome of patients with acute left ventricular failure prospective study. Int J Adv Med. 2020;7(05):764-769.
- [Google Scholar]
- Lung ultrasound for the evaluation of pulmonary congestion in outpatients: a comparison with clinical assessment, natriuretic peptides, and echocardiography. JACC Cardiovasc Imaging. 2013;6(11):1141-1151.
- [Google Scholar]
- Prognostic value of residual pulmonary congestion at discharge assessed by lung ultrasound imaging in heart failure. Eur J Heart Fail. 2015;17(11):1172-1181.
- [Google Scholar]
- Combination of lung ultrasound (a comet-tail sign) and N-terminal pro-brain natriuretic peptide in differentiating acute heart failure from chronic obstructive pulmonary disease and asthma as cause of acute dyspnea in prehospital emergency setting. Crit Care. 2011;15(02):R114.
- [Google Scholar]
- Detection and prognostic value of pulmonary congestion by lung ultrasound in ambulatory heart failure patients. Eur Heart J. 2016;37(15):1244-1251.
- [Google Scholar]
- Prognostic value of lung ultrasound in chronic stable ambulatory heart failure patients. Rev Esp Cardiol (Engl Ed). 2021;74(10):862-869.
- [Google Scholar]
- Gender difference in the prognostic value of N-terminal pro-B type natriuretic peptide in patients with heart failure—a report from the Korean Heart Failure Registry (KorHF) J-Stage. 2017;81(09):1329-1336.
- [Google Scholar]
- Integrative assessment of congestion in heart failure throughout the patient journey. JACC Heart Fail. 2018;6(04):273-285.
- [Google Scholar]
- Expert consensus document: reporting checklist for quantification of pulmonary congestion by lung ultrasound in heart failure. Eur J Heart Fail. 2019;21(07):844-851.
- [Google Scholar]







