Translate this page into:
An Observational Study: Ambulatory Blood Pressure Monitoring after Percutaneous Transluminal Coronary Angioplasty
Gopi Krishna Kenchi, MD (DM) Department of Cardiology Nizam's Institute of Medical Sciences, Punjagutta, Hyderabad 500082, Telangana India drgopikrishna44@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Aim In recent studies, lack of fall in nocturnal blood pressure (BP) has been presented as an independent predictor of poor prognosis. The aim of this study is to investigate the prognostic value of various variables of BP by 24-hour ambulatory blood pressure (ABP) measurement and sex-related differences after percutaneous transluminal coronary angioplasty (PTCA).
Methods This study included 100 patients who underwent PTCA in the authors’ institute from June 2017 to January 2018. They were monitored by 24-hour ABP for 1 day in the hospital.
Results One hundred patients were recruited in this study with mean age of 61.64 years, with female-to-male ratio of 0.27:1. All demographic, clinical, and laboratory parameters including the ABP parameters were comparable between females and males, except smoking and alcoholism that were more frequent in males.
Out of 100 patients, 41 had nocturnal dipping in BP and 59 did not have nocturnal dipping. In this study, the variables among nondippers, 16 (27.1%) were females, 43 (72.8%) were males, 45 (63.3%) had diabetes mellitus (DM), 46 (75.4%) had hypertension (HTN), mean systolic blood pressure (SBP) was 141.7 ± 13.9 mm Hg, mean diastolic blood pressure (DBP) was 86.34 ± 5.64 mm Hg, mean pulse pressure (PP) was 55.39 ± 9.25 mm Hg, and pulse-wave velocity (PWV) was 6.69 ± 2.22 m/s.
In females were more nondippers (27.1%) than dippers (12.1%), which was statistically significant (p = 0.05). Nondippers were more among hypertensive patients (77.9% vs. 36.5%; p = 0.00). Higher mean SBP (p = 0.001), higher mean BP (p = 0.032), and higher mean pulse pressure (p = 0.00) were observed in nondippers.
However, age, ejection fraction (EF), presence of DM, coronary artery disease (CAD) severity, type of presentation, and PWV were not different in dipper versus nondippers. Conclusion With comparable clinical, laboratory parameters along with BP parameters between females and males, immediate post-percutaneous coronary intervention (PCI) patients, female PCI patients had more nondippers (p = 0.05). Overall nondippers had higher SBP, mean BP, and PP than dippers. Diabetes, severity of CAD, and type of presentation of CAD (as ACS or CSA) did not influence the nocturnal dipping quality of the BP.
Keywords
ambulatory blood pressure monitoring
coronary artery disease
percutaneous transluminal coronary angioplasty
Introduction
In the past decade, there has been an explosive growth of ambulatory blood pressure (ABP) monitoring for clinical purposes and research.1 2 Several outcome studies have been published, particularly during the past few years.1 2 3 4 5 6 7 8 9 10 11 13 14 15 16 17 18 19 20 21 22 23 24 25 These studies were conducted in the general population19 20 or in hypertensive subjects, who were either untreated3 4 5 6 7 8 9 10 11 12 13 14 16 or treated15 17 18 at the time of ABP monitoring. The general result of these studies was that the difference in the cardiovascular disease (CVD) risk between categories generated by one session of ABP monitoring was greater than the difference in the risk between categories generated by one or a few standard office blood pressure (BP) measurements.
The aim of this study was to investigate the prognostic value of various variables of BP obtained by 24-hour ABP measurement and sex-related differences after percutaneous transluminal coronary angioplasty (PTCA).
Methods
This was a prospective, observational, and single-center study. This study was conducted in the department of cardiology at our institute. This study included 100 consecutive patients who underwent PTCA in our institute from June 2017 to January 2018 irrespective of presence or absence of hypertension (HTN). This study was approved by the institutional review board. An informed written consent was obtained from the participants before recruiting them in this study. Major exclusion criteria were patients having hemodynamic instability requiring intraaortic balloon pump (IABP) or inotropic support or mechanical ventilation, insomnia, and arrhythmia that interfere with ABP monitoring devices. Baseline data regarding age, sex, and conventional coronary artery disease (CAD) risk factors (diabetes mellitus [DM], HTN, and smoking) were collected. Diagnosis and indication for percutaneous coronary intervention (PCI) were recorded. All patients were subjected to undergo routine blood investigations, including complete blood counts, blood sugar, liver function tests (LFT), lipid profile, blood urea, serum creatinine, and serum electrolytes. Electrocardiogram (ECG) and transthoracic echocardiography were performed for all patients. They were monitored by ABP for 24 hours in the hospital.
Ambulatory Blood Pressure Monitoring
The 24-hour ABP measurement was performed using a portable compact digital recorder (Tonoport V, GE Health-care) and an analyzer using customized analytical software programmed to measure BPs at 15-minute intervals during day time from 07:00 until 23:00, and at 30-minute intervals during night time from 23:00 until 07:00. The patients were instructed to perform their routine daily activities, but to stay inactive during the measurements. Recordings were accepted if more than 80% of the raw data were valid. The inflatable cuff was always placed on the nondominant upper limb.
The analyzed variables included the following: mean SBP, mean DBP, mean PP, mean pulse-wave velocity (PWV), and presence or absence of dipping.
Results
The demographic details of the study were given in Table 1 and Fig. 1.

-
Fig. 1 Sex distribution of the study population.
Fig. 1 Sex distribution of the study population.
|
Variable |
Number |
|---|---|
|
Abbreviations: ACS, acute coronary syndrome; CSA, chronic stable angina; DM, diabetes mellitus; HTN, hypertension. |
|
|
Age (y) |
61.64 ± 8.50 |
|
Females |
21 (21%) |
|
Males |
79 (79%) |
|
DM |
71 (71%) |
|
HTN |
61 (61%) |
|
Smoking |
31 (31%) |
|
ACS |
59 (59%) |
|
CSA |
41 (41%) |
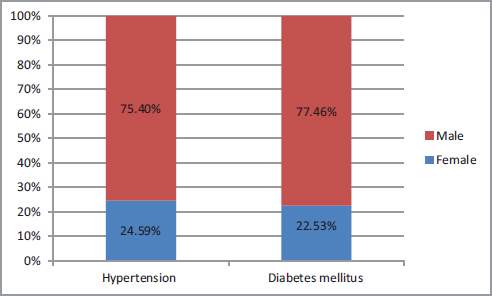
Out of 100 patients, 21 (21%) were females and 79 (79%) were males (Fig. 1). Mean age of study population is 61.64 ± 8.50 years. Overall, 61 (61%) patients had HTN, 71 (71%) had DM, and 31 (31%) had a history of smoking (Fig. 2). The most common presentation in our study was acute coronary syndrome (ACS) (59%) that comprises unstable angina, non–ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI).
-
Fig. 2 Sex distribution among diabetes mellitus and hypertension.
Fig. 2 Sex distribution among diabetes mellitus and hypertension.
Table 2 compares baseline characteristics based on sex. Both the groups were comparable regarding age, DM, HTN, number of stents, mean EF, and number of diseased vessels, except male patients who were more likely to have history of alcohol consumption and smoking. Mean age did not differ significantly between female and male patients (62.48 ± 7.88 years vs. 61.4 ±8.7 years, p = 0.59) (Fig. 3). The mean EF among female patients was 56.3 ± 10.31% and among male patients was 52.65 ± 10.85% (p = 0.15), which is not statistically significant (p = 0.15).

-
Fig. 3 Age comparison between males and females.
Fig. 3 Age comparison between males and females.
|
Variable |
Female (mean ± SD) |
Male (mean ± SD) |
p Value |
|---|---|---|---|
|
Abbreviations: CAG, coronary angiography; SD, standard deviation. |
|||
|
Age (y) |
62.48 ± 7.88 |
61.42 ± 8.70 |
0.59 |
|
Hypertension (%) |
15 (24.59%) |
46 (75.40%) |
0.24 |
|
Diabetic mellitus (%) |
16 (22.53%) |
55 (77.46%) |
0.53 |
|
Smoking (%) |
1 (4.7%) |
32 (40.5%) |
0.00 |
|
Alcoholism (%) |
0 |
33 (42.3%) |
0.00 |
|
Stents (no. per patient) |
2.00 ± 0.71 |
1.77 ± 0.60 |
0.18 |
|
Ejection fraction (%) |
56.33 ± 10.31 |
52.65 ± 10.85 |
0.15 |
|
CAG (single vs. multi) |
12 (57.1%) |
52 (65.8%) |
0.47 |
From the ABP monitoring different variables were noted. No significant differences in various parameters obtained from ABP were noted between male and female patients. Mean BP of female and male patients was identical (104.19 ± 9.54 vs 102.33 ± 12.72 mm Hg, p = 0.46). The average PWV among female patients was 7.06 ± 2.18 m/s, and among male patients it was 6.72 ± 2.52 m/s, which was not statistically significant (p = 0.54). Statistically significant sex difference was not there even in mean systolic blood pressure (SBP), mean diastolic blood pressure (DBP), and pulse pressure (PP) (Table 3). The mean heart rate (HR) among female and male patients was similar (71.95 ± 19.12 vs. 72.66 ± 17.22 beats/min, p = 0.87) (Table 2).
|
Variable |
Female (mean ± SD) |
Male (mean ± SD) |
p Value |
|---|---|---|---|
|
Abbreviations: ABP, ambulatory blood pressure. |
|||
|
Mean systolic blood pressure (mm Hg) |
140.76 ± 17.20 |
135.77± 16.66 |
0.24 |
|
Mean diastolic blood pressure (mm Hg) |
85.33 ± 6.04 |
85.09 ± 11.36 |
0.89 |
|
Average mean blood pressure (mm Hg) |
104.19 ± 9.54 |
102.33 ± 12.72 |
0.46 |
|
Mean pulse pressure (mm Hg) |
55.43 ± 11.97 |
50.68 ± 8.69 |
0.10 |
|
Mean heart rate (beats/min) |
71.95 ± 19.12 |
72.66 ± 17.22 |
0.87 |
|
Pulse-wave velocity (m/s) |
7.06 ± 2.18 |
6.725 ± 2.52 |
0.54 |
|
Maximum systolic blood pressure (mm Hg) |
166.95 ± 8.16 |
164.54 ± 6.40 |
0.22 |
|
Maximum diastolic blood pressure (mm Hg) |
110.95 ± 5.58 |
112.81 ± 6.97 |
0.20 |
|
Minimum systolic blood pressure (mm Hg) |
112.86 ± 8.82 |
109.84 ± 9.28 |
0.17 |
|
Minimum diastolic blood pressure (mm Hg) |
61.38 ± 9.01 |
59.93 ±7.05 |
0.50 |
Among 100 patients, 41 (41%) patients had nocturnal dipping and 59 (59%) did not have nocturnal dipping. When comparing the different demographic, clinical, and laboratory parameters between nocturnal dippers and blunted dippers, female patients were more likely to have nondipping (p = 0.05). Patients with prior history of HTN had nondipping nocturnal BP compared with prior normotensive patients (77.9% vs. 36.5%, p = 0.001). Nondippers had higher 24 hours mean SBP (p = 0.001), 24-hours mean BP (p = 0.032), and 24-hours mean PP compared with dippers, which was statistically significant (p = 0.00) (Table 4, Fig. 4). However, there was no significant difference in 24-hour mean HR and 24-hours mean PWV between dippers and nondippers. Mean age, mean EF, presence of DM, CAD severity, and type of presentation were not different in dipper versus nondippers (Fig. 5).

-
Fig. 4 Statistically significant variables (p < 0.05) in dippers and non-dippers in females.
Fig. 4 Statistically significant variables (p < 0.05) in dippers and non-dippers in females.

-
Fig. 5 Statistically insignificant variables (p > 0.05) in dippers and nondippers in males.
Fig. 5 Statistically insignificant variables (p > 0.05) in dippers and nondippers in males.
|
Variables |
Nondippers (mean ± SD) |
Dippers (mean ± SD) |
p Value |
|
|---|---|---|---|---|
|
Abbreviations: ACS, acute coronary syndrome; CAD, coronary artery disease; CSA, chronic stable angina; DBP, diastolic blood pressure; DM, diabetes mellitus; DVD, double-vessel disease; EF, ejection fraction; HR, heart rate; HTN, hypertension; MBP, mean blood pressure; PP, pulse pressure; PWV, pulse-wave velocity; SBP, systolic blood pressure; SVD, single-vessel disease. |
||||
|
Age |
62.78 ± 7.93 |
60.00 ± 9.13 |
0.118 |
|
|
EF |
53.2 ± 10.2 |
53.8 ± 11.7 |
0.788 |
|
|
Females |
16 (27.1%) |
5 (12.1%) |
0.05 |
|
|
Males |
43 (72.8%) |
36 (87.8%) |
0.08 |
|
|
DM |
45 (76.27%) |
26 (63.4%) |
0.16 |
|
|
HTN |
46 (77.9%) |
15 (36.5%) |
0.001 |
|
|
CAD |
SVD |
29 (70.7%) |
35 (59.3%) |
0.23 |
|
DVD |
12 (29.2%) |
24 (40.6%) |
0.23 |
|
|
Presentation |
CSA |
15 (36.5%) |
26 (44.06%) |
0.45 |
|
ACS |
26 (63.4%) |
33 (55.9%) |
0.45 |
|
|
Stents |
1 |
15 (25.4%) |
16 (39.02%) |
0.15 |
|
2 |
34 (57.6%) |
23 (56.09%) |
0.87 |
|
|
3 |
10 (16.9%) |
2 (4.8%) |
0.042 |
|
|
Mean SBP |
141.7 ± 13.9 |
129.8 ± 18.3 |
0.001 |
|
|
Mean DBP |
86.34 ± 5.64 |
83.4 ± 14.8 |
0.234 |
|
|
Mean MBP |
105.12 ± 8.20 |
99.3 ± 15.6 |
0.032 |
|
|
Mean PP |
55.39 ± 9.25 |
46.34 ± 7.42 |
0.000 |
|
|
Mean HR |
73.0 ± 16.9 |
71.8 ± 18.6 |
0.735 |
|
|
PWV |
6.69 ± 2.22 |
6.94 ± 2.76 |
0.637 |
|
Discussion
Arterial BP exhibits a diurnal rhythm that is higher at daytime than at nighttime.26 27 28 A nocturnal fall in BP of less than 10% of the daytime value has been termed as “nondippers.”29 Continuous 24-hour ABP monitoring has been used to show the diurnal rhythm of arterial BP. The mechanisms responsible for abnormal diurnal variation in BP remain unclear, but it may be associated with an autonomic balance deterioration.30 Erdem et al reported a possible cardiac autonomic dysfunction in prehypertensive, nondipper patients.31 Verdecchia et al demonstrated that lack of nocturnal decline in BP in patients with essential HTN was a good predictor of cardiovascular prognosis.5 Furthermore, nondipper pattern is a predictor of target organ damage, including stroke, renal failure, and adverse cardiovascular events.32 33 34 Kang et al reported that CAD patients often had lack of nocturnal BP fall, which might increase the future coronary events risk, including ACS.35 Zain-El et al reported that in elderly patients with isolated systolic HTN nondipping morning BP was an independent predictor of hypertensive target organ damage.36 Cha et al reported that masked and sustained HTN and nondipping or reverse dipping pattern were more common in patients with severe renal failure and proteinuria.37 Karakas et al demonstrated the nondipping BP pattern relation with impaired left ventricular dyssynchrony in dipper and nondipper hypertensives.38
In our study, we observed that women had blunted nocturnal dipping (p = 0.05) when compared with men (p = 0.08). This finding is consistent with previous study reports by Sherwood et al,39 which concluded that women with CAD may be exposed to a higher nocturnal BP, which could put them at higher risk for further target organ damage and adverse clinical outcomes. They also noted that ambulatory PP was elevated during both the daytime and nighttime in women with CAD. They also showed that CAD and advancing age were associated with blunted nocturnal BP dipping in women. In the PIUMA (Progetto Ipertensione Umbria Monitoraggio Ambulatoriale) study, hypertensive women with nondipping pattern at the baseline evaluation had a higher cardiovascular morbidity rate during follow-up than dippers, and this difference remained significant even after control for traditional risk factors. A nonsignificant trend in the same direction was found in men.5
A recent study by Cicek et al40 observed that 56 (66.66%) patients had nondipper pattern and 28 (33.33%) had dipper pattern. They observed a significant difference in CF-PWV (nondipper vs. dipper; 8.91 ± 2.53 vs. 7.66 ± 1.08 m/s, p = 0.002), female sex (55% vs. 32%, p = 0.045), and nocturnal BP measurements (for mean BP; 106 ± 11 vs. 92 ± 8 mm Hg, p < 0.001). By multiple logistic regression analysis, they revealed female sex (p = 0.021), nocturnal mean BP (p < 0.001), and CF-PWV (p = 0.004) as the independent predictors of nondipper hypertensive pattern. Nondipper pattern, mainly related to increased PWV and impaired modulation of vascular smooth muscle tone during the night, may justify an increased cardiovascular risk in these patients.
This study results were consistent with those of our study in terms of female sex (nondippers vs. dippers; 27% vs. 12%, p = 0.05) and high mean BP (105.12 ± 8.20 vs. 99.3 ± 15.6 mm Hg, p = 0.032). However, in contrast PWV was not statistically significant between the two groups (6.69 ± 2.22 vs. 6.94 ± 2.76, p = 0.637).
In our study, we found the statistically higher 24-hour PP in nondippers than dippers (p = 0.00). This finding was consistent with previous study reports by Verdecchia et al,10 which concluded that ambulatory PP was a potent independent predictor of total cardiovascular risk in initially untreated essential hypertensive white patients. Ambulatory PP was a more accurate marker than office PP of increased arterial stiffness or already diseased arteries.41 In CAD patients there was an association between a higher PP and cardiac events.42 The elevated PP was a result of increased conduit vessel stiffness. Furthermore, it was likely that the increased load associated with conduit vessel stiffening contributed to a reduction in stroke volume in the patients with increased PP. The stiffness of Conduit vessel increased the amplitude of PP produced by a given flow wave, resulting in higher systolic and lower diastolic pressures for any given mean pressure. In stiffened conduit vessels PWV was increased, and this shortened the time required for the forward pressure wave to travel down the aorta and peripheral conduits to the various reflecting sites and back to the heart. The resulting movement of the reflected wave into systole from diastole has no effect on mean arterial pressure (MAP). However, the premature reflected wave further increases the systolic pressure-time integral and decreases the diastolic pressure-time integral, thereby increasing systolic load while decreasing coronary perfusion pressure.
Conclusion
With comparable clinical, laboratory parameters along with BP parameters between females and males, immediate post-PCI patients and female PCI patients had more nondippers (p = 0.05). Overall nondippers had higher SBP, mean BP, and PP than dippers. Diabetes, severity of CAD, and type of presentation of CAD (as ACS or CSA) did not influence the nocturnal dipping quality of the BP.
Limitations of the Study
This study provided no information regarding long-term clinical outcomes. It was a nonrandomized study from a single center.
Conflict of Interest
None.
References
- American Society of Hypertension Ad Hoc Panel. Recommendations for the use of home (self) and ambulatory blood pressure monitoring. Am J Hypertens. 1996;9(01):1-11.
- [Google Scholar]
- Clinical value of ambulatory blood pressure monitoring. J Hypertens. 1999;17(05):585-595.
- [Google Scholar]
- Prognostic value of ambulatory blood pressure measurements: further analyses. J Hypertens Suppl. 1989;7(03):S3-S10.
- [Google Scholar]
- Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24(06):793-801.
- [Google Scholar]
- Nocturnal pressure is the true pressure. Blood Press Monit. 1996;1:S81-S85. Suppl 2
- [Google Scholar]
- Prognostic significance of blood pressure variability in essential hypertension. Blood Press Monit. 1996;1(01):3-11.
- [Google Scholar]
- Prognostic significance of the white coat effect. Hypertension. 1997;29(06):1218-1224.
- [Google Scholar]
- Adverse prognostic value of a blunted circadian rhythm of heart rate in essential hypertension. J Hypertens. 1998;16(09):1335-1343.
- [Google Scholar]
- Ambulatory pulse pressure: a potent predictor of total cardiovascular risk in hypertension. Hypertension. 1998;32(06):983-988.
- [Google Scholar]
- Altered circadian blood pressure profile and prognosis. Blood Press Monit. 1997;2(06):347-352.
- [Google Scholar]
- Blunted nocturnal fall in blood pressure in hypertensive women with future cardiovascular morbid events. Circulation. 1993;88(03):986-992.
- [Google Scholar]
- Cardiovascular outcome in white-coat versus sustained mild hypertension: a 10-year follow-up study. Circulation. 1998;98(18):1892-1897.
- [Google Scholar]
- “Non- dipping” related to cardiovascular events in essential hyper-tensive patients. Acta Med Austriaca. 1994;21(03):86-89.
- [Google Scholar]
- Systolic Hypertension in Europe Trial Investigators. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. JAMA. 1999;282(06):539-546.
- [Google Scholar]
- Adverse effect of nighttime blood pressure on the outcome of lacunar infarct patients. Stroke. 1998;29(03):570-576.
- [Google Scholar]
- Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: a prospective study. Hypertension. 1998;31(02):712-718.
- [Google Scholar]
- Prognostic value of ambulatory and home blood pressure measurements in comparison to screening blood pressure measurements: a pilot study in Ohasama. Blood Press Monit. 1996;1(02):S51-S58.
- [Google Scholar]
- Prediction of mortality by ambulatory blood pressure monitoring versus screening blood pressure measurements: a pilot study in Ohasama. J Hyper-tens. 1997;15(04):357-364.
- [Google Scholar]
- Clinical value of ambulatory blood pressure: evidence and limits. Circ Res. 2015;116(06):1034-1045.
- [Google Scholar]
- Cardiovascular risk in hypertension in relation to achieved blood pressure using automated office blood pressure measurement. Hypertension. 2016;68(04):866-872.
- [Google Scholar]
- Role and relevance of blood pressure variability in hypertension related co-morbidi-ties. J Assoc Physicians India. 2017;65(12):83-92.
- [Google Scholar]
- Prevalence and clinical outcomes of white-coat and masked hypertension: analysis of a large ambulatory blood pressure database. J Clin Hypertens (Greenwich). 2018;20(02):297-305.
- [Google Scholar]
- Night-time heart rate nondipping: clinical and prognostic significance in the general population. J Hypertens. 2018;36(06):1311-1317.
- [Google Scholar]
- Variation in arterial pressure throughout the day and night. Clin Sci. 1964;26:445-460.
- [Google Scholar]
- Brain renin-angiotensin system in hypertension, cardiac hypertrophy, and heart failure. Front Physiol. 2012;2:115.
- [Google Scholar]
- Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990;81(02):528-536.
- [Google Scholar]
- Impaired diurnal blood pressure variation and all-cause mortality. Am J Hypertens. 2008;21(01):92-97.
- [Google Scholar]
- Cardiac autonomic function measured by heart rate variability and turbulence in pre-hypertensive subjects. Clin Exp Hypertens. 2013;35(02):102-107.
- [Google Scholar]
- Relation between nocturnal decline in blood pressure and mortality. The Ohasama study. Am J Hypertens. 1997;10(11):1201-1207.
- [Google Scholar]
- Increase in nocturnal blood pressure and progression to microalbuminuria in type 1 diabetes. N Engl J Med. 2002;347(11):797-805.
- [Google Scholar]
- Association of impaired diurnal blood pressure variation with a subsequent decline in glomerular filtration rate. Arch Intern Med. 2006;166(08):846-852.
- [Google Scholar]
- Ambulatory blood pressure monitoring in the prediction and prevention of coronary heart disease. Curr Hypertens Rep. 2013;15(03):167-174.
- [Google Scholar]
- Non-dipping morning blood pressure and isolated systolic hypertension in elderly. Bratisl Lek Listy (Tlacene Vyd). 2013;114(03):150-154.
- [Google Scholar]
- Association between blood pressure and target organ damage in patients with chronic kidney disease and hypertension: results of the APrODiTe study. Hypertens Res. 2014;37(02):172-178.
- [Google Scholar]
- Assessment of left ventricular dyssynchrony in dipper and non-dipper hypertension. Blood Press. 2013;22(03):144-150.
- [Google Scholar]
- Nighttime blood pressure dipping in postmenopausal women with coronary heart disease. Am J Hypertens. 2012;25(10):1077-1082.
- [Google Scholar]
- Non-dipping pattern in untreated hypertensive patients is related to increased pulse wave velocity independent of raised nocturnal blood pressure. Blood Press. 2013;22(01):34-38.
- [Google Scholar]
- J-shaped relation between change in diastolic blood pressure and progression of aortic atherosclerosis. Lancet. 1994;343:504-507. 8896
- [Google Scholar]
- Sphygmomanometrically determined pulse pressure is a powerful independent predictor of recurrent events after myocardial infarction in patients with impaired left ventricular function. SAVE investigators. Survival and ventricular enlargement. Circulation. 1997;96(12):4254-4260.
- [Google Scholar]







