Translate this page into:
Additional Heart Sounds—Part 1 (Third and Fourth Heart Sounds)
Ramya Pechetty, MD, DM Department of Cardiology, Apollo Hospitals Jubilee Hills, Hyderabad India ramyapechetty@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
S3 is a low-pitched sound (25–50Hz) which is heard in early diastole, following the second heart sound. The following synonyms are used for it: ventricular gallop, early diastolic gallop, protodiastolic gallop, and ventricular early filling sound. The term “gallop” was first used in 1847 by Jean Baptiste Bouillaud to describe the cadence of the three heart sounds occurring in rapid succession. The best description of a third heart sound was provided by Pierre Carl Potain who described an added sound which, in addition to the two normal sounds, is heard like a bruit completing the triple rhythm of the heart (bruit de gallop). The following synonyms are used for the fourth heart sound (S4): atrial gallop and presystolic gallop. S4 is a low-pitched sound (20–30 Hz) heard in presystole, i.e., shortly before the first heart sound. This produces a rhythm classically compared with the cadence of the word “Tennessee.” One can also use the phrase “A-stiff-wall” to help with the cadence (a S4, stiff S1, wall S2) of the S4 sound.
Keywords
ventricular gallop
protodiastolic gallop
physiological S3
pathological S3
atrial gallop
presystolic gallop
Third Heart Sound (S3)
Definition
S3 is an early diastolic sound. It is a low-pitched sound (25–50Hz) that occurs after the second heart sound. It produces a rhythm like the cadence of the word “Kentucky” in which “CKY” represents S3.
Synonyms
Ventricular gallop, early diastolic gallop, protodiastolic gallop, ventricular early filling sound.
History
S3 was first described in 1847 by Jean Baptiste Bouillaud who referred to it as a gallop. Pierre Carl Potain described S3 as an additional sound like a bruit, completing the triple rhythm of the heart (bruit de gallop).1 The phrase “Slosh-ing-IN” can also be used to describe the S1-S2-S3 sounds.
Physiology
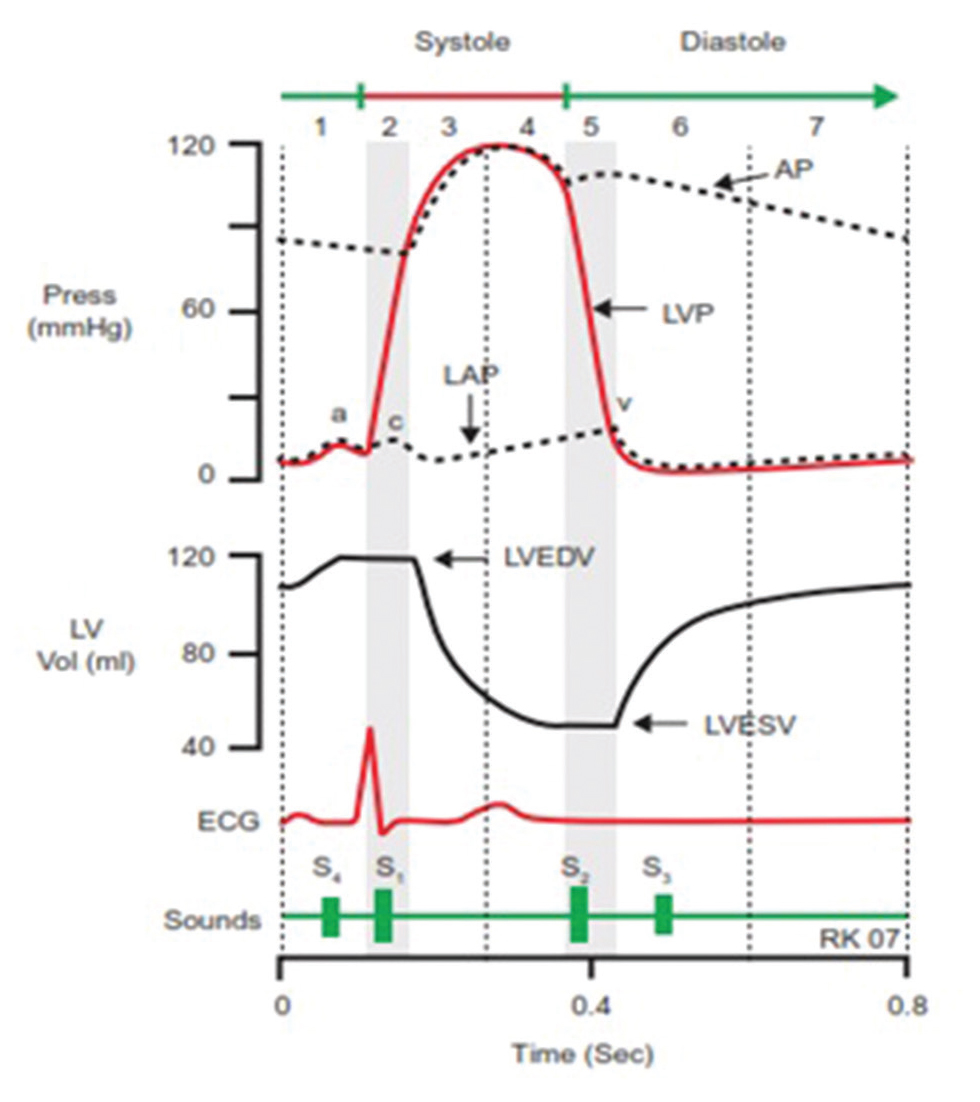
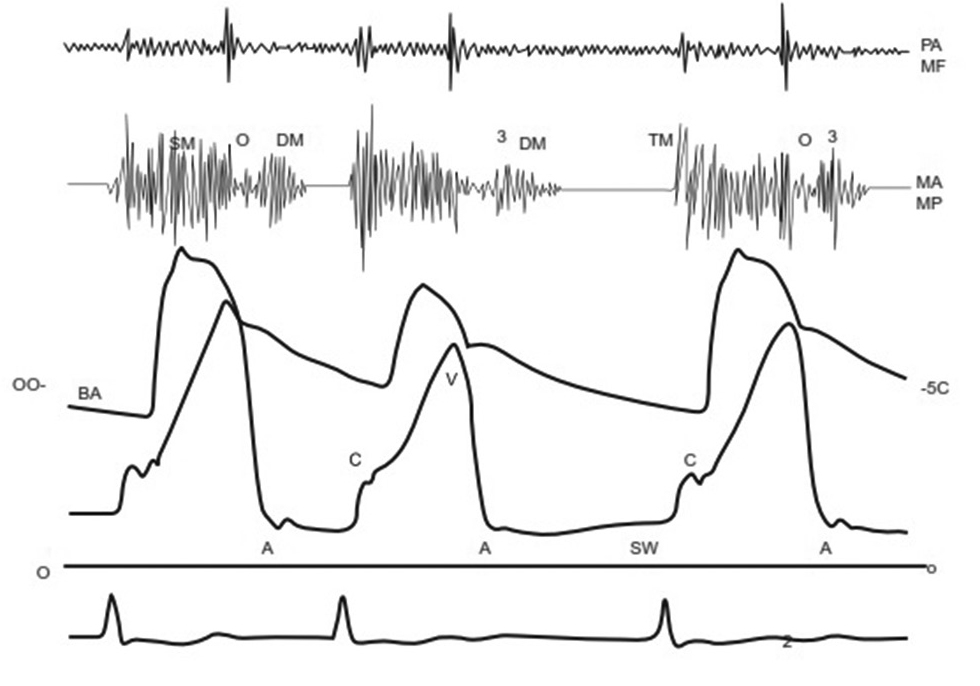
In early diastole, when ventricular pressure falls below the atrial pressure, the atrioventricular valves open wide, and blood drains rapidly from the atria (Y descent) into the ventricles, producing S3 (Fig. 1). S3 occurs at the beginning of the middle third of ventricular diastole, i.e., at the end of rapid filling phase. In fact, it represents the transition from rapid filling to slow filling phase of the ventricles. It does not occur with the beginning of diastole, because the ventricles are not sufficiently filled to create any reverberation till the middle third in a normal heart.
-
Fig. 1 Cardiac cycle showing the association of S3 with the early filling phase.
Fig. 1 Cardiac cycle showing the association of S3 with the early filling phase.
Mechanism
The exact mechanism of genesis of S3 is debatable. The probable theories are as follows:
-
Ventricular theory–The rapid filling in early diastole distends the ventricles. When the elastic distensibility of the ventricular wall is reached, there is sudden deceleration of the inflowing blood with attendant vibration of the “cardio-hemic” system.2 3 4 S3 is thought to be an intracardiac sound arising from the vibration of ventricular wall as the diastolic inflow is suddenly halted.
-
Valvular theory–It is proposed that S3 is the result of vibrations of valve cusps rather than the ventricular wall when the diastolic inflow is suddenly decelerated.
However, recent studies have shown that the third heart sound is heard loudest external to the left ventricular cavity, implying it to be extra-cardiac in origin.
-
Impact theory–S3 results from movement of ventricle closer to the chest wall. When the ventricle is dilated, it lies in proximity to the chest wall. When blood enters during diastole, it results in a more forceful impact producing S3.5 6 7
-
S3 may arise within the ventricular apex due to sudden limitation of longitudinal expansion of the ventricle after early rapid filling.8 9
Thus, S3 can be heard in the following three situations:
-
Normal ventricle receiving excessive volume of incoming blood (e.g., hyperdynamic states).
-
Dilated ventricle that is stretched and overfilled receiving relatively normal or less than normal amount of blood (e.g., systolic dysfunction).
-
Dilated ventricle received more blood, that is, diastolic volume overload (e.g., LV in ventricular septal defect [VSD], patent ductus arteriosus [PDA], mitral regurgitation [MR]; RV in tricuspid regurgitation [TR], atrial septal defect [ASD]).
Prerequisites for Genesis of S3
-
Atria–Atrial pressure.
-
Unobstructed AV valves.
-
Ventricles–Early diastolic relaxation and distensibility of the ventricles.
-
Blood volume.
-
Degree of contact with the chest wall.
Force of delivery of the blood into the ventricle, and the ability of the ventricles to accept are the most important factors influencing the occurrence of S3.
Absent S3
-
Pericardial tamponade.
-
Mitral or tricuspid stenosis.
-
Obesity, thick chest wall, and lung disease.
-
Mild LV dysfunction.
-
Diuresis or excess volume depletion.
Clinical Recognition of S310 11 12:
S3 is a low-pitched sound heard 120 to 200 milliseconds after A2. It can be of left or right ventricular origin. Characteristic features of LV S3 and RV S3 are mentioned in Table 1.
|
Characteristic features |
LV S3 |
RV S3 |
|---|---|---|
|
Abbreviation: IJV, internal jugular vein. |
||
|
Site of audibility |
Apex |
Lower left sternal border, epigastrium, rarely over the jugular veins (right IJV as it is in line with RA and RV) |
|
Effect of respiration |
Breath-holding in expiration enhances audibility |
Better heard in inspiration |
|
Position of patient |
Supine position, 30°left lateral position with the left arm extended upward away from the chest. |
Supine position with passive leg raising. |
|
Isometric hand grip |
Increases the intensity |
No change |
|
Associated features |
Left sided causes for S3 |
Raised JVP, usually prominent Y descent |
-
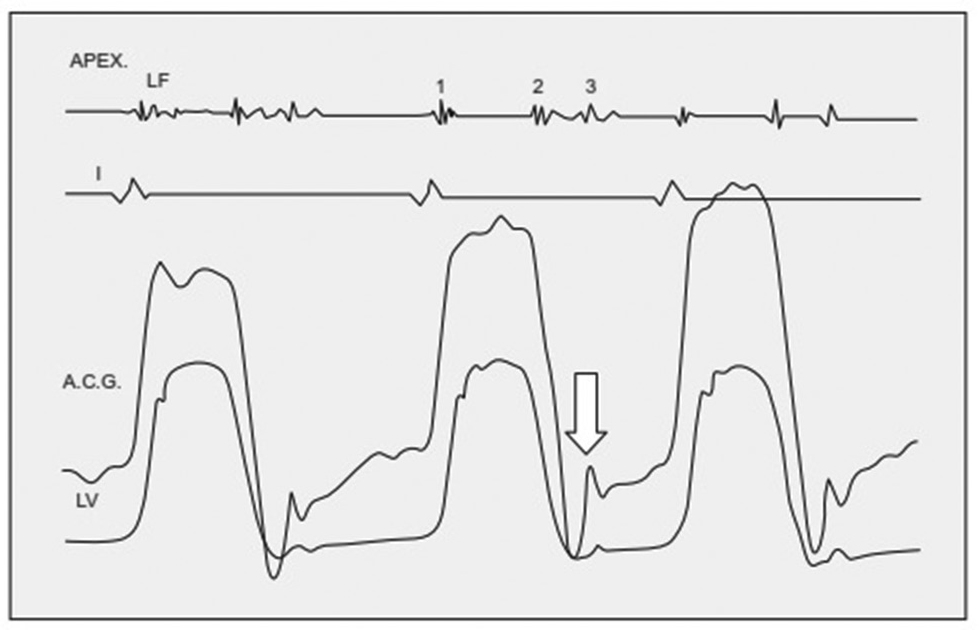
S3 corresponds to the rapid filling wave in the apex cardiogram (ACG) (Fig. 2).
-
S3 is often the most difficult heart sound to hear because it is exceptionally low in intensity and is easily obscured by extraneous sounds in the room. The patient should be examined in a quiet room in supine position.
-
S3 is best heard with the bell of the stethoscope placed lightly.
-
Simultaneous palpation and inspection of the apex should be done.
-
The third heart sound may rarely be palpable and/or visible just after the apical impulse such as in a young individual with thin chest wall.
-
A third heart sound is rarely palpable or visible when not audible.
-
Inspiratory increase in RV S3 is absent in conditions of right ventricular distention or failure, where inspiratory augmentation of venous return does not occur.
-
Intensity of RV S3 is increased by techniques that increase venous return or the size of the ventricular cavity, such as recumbent position, elevation of the legs, and volume expansion. Conversely, S3 becomes softer or disappears with standing, diuresis, hemorrhage, or dialysis.
-
Fig. 2 ACG in a patient with heart failure showing rapid filling wave or palpable S3 (arrow). ACG, apex cardiogram.
Fig. 2 ACG in a patient with heart failure showing rapid filling wave or palpable S3 (arrow). ACG, apex cardiogram.
Differential Diagnosis
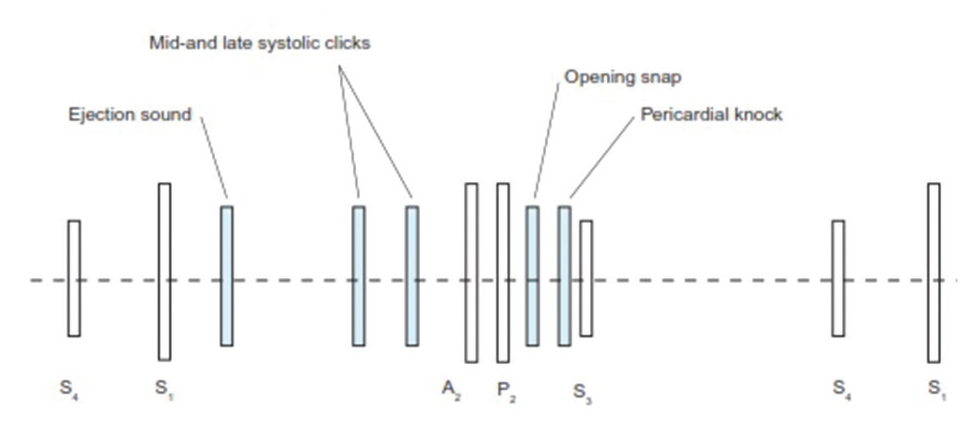
S3 must be differentiated from other diastolic sounds (Table 2 Fig. 3).
|
Heart sound |
Timing after A2 |
Pitch |
Site |
Associated features |
|---|---|---|---|---|
|
Abbreviations: LLSB, lower left sternal border; MDM, mid diastolic murmur; MR, mitral regurgitation. |
||||
|
S3 |
0.12–0.20 second |
Low |
Apex/LLSB |
Cardiomegaly, raised JVP, MR murmur |
|
S4 |
Precedes S1 |
Low, slightly more than S3 |
Apex/LLSB |
Open palpable |
|
Split S2 |
0.04–0.12sec |
Medium to high |
upper left sternal border |
Varies with respiration |
|
Opening snap |
0.04–0.12 second |
Medium to high |
LLSB/Apex |
Loud S1, MDM of mitral stenosis |
|
Tumor plop |
0.08–0.13 second |
Low |
Apex |
Varies with position |
|
Pericardial knock |
0.09–0.12 second |
Medium to high |
Apex |
Features of constriction |
-
Fig. 3 Relationship of diastolic sounds to S1 and S2.
Fig. 3 Relationship of diastolic sounds to S1 and S2.
Causes
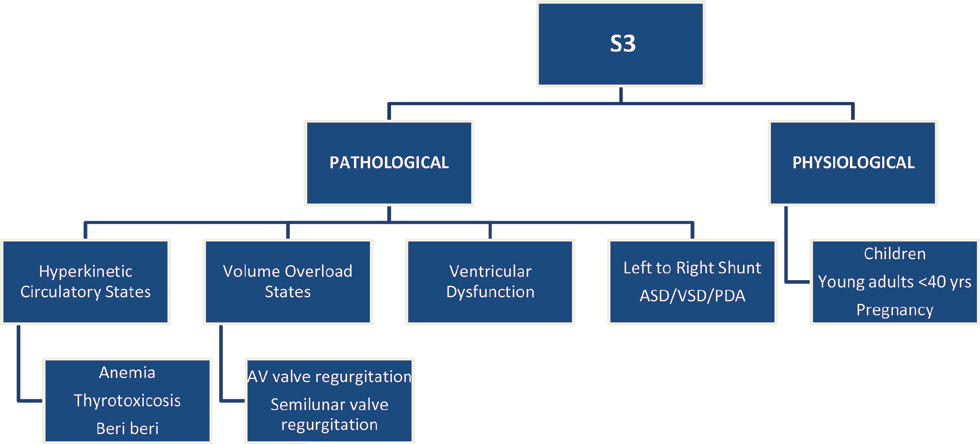
S3 can be right or left ventricular in origin (Fig. 4).
-
Fig. 4 Causes of S3.
Fig. 4 Causes of S3.
Clinical Significance of S3
physiological or pathological–S3 can be appreciated normally in children and adults younger than 40 years of age, owing to the presence of a compliant ventricle with increased early diastolic filling rate and a thin chest wall. The disappearance of the physiologic S3 with age results from a decrease in early diastolic left ventricular filling and subsequent deceleration of inflow due to the development of relative left ventricular hypertrophy in adulthood.13
A third heart sound after the age of 40 years is usually abnormal and suggests ventricular dysfunction or volume overload.
Although there are no distinctive features to differentiate physiological and pathological S3, the following features favor a pathological S3;
-
Presence of cardiomegaly.
-
Louder S3.
-
Earlier S3.
Pathological S3
Hyperkinetic Circulatory States
-
S3 can be heard in severe anemia, thyrotoxicosis, beriberi, complete A–V block, renal failure, systemic AV fistula, and volume overload from excessive fluids or blood transfusion.
-
S3 in these conditions is due to increased blood volume into a normal sized ventricle.
-
S3 can also.. be appreciated in athletes owing to slow heart rates and increased filling volumes.14
-
A third heart sound in the above-mentioned conditions does not indicate LV dysfunction.15
S3 in Shunt Lesions
-
Increased blood flow and rapid early diastolic filling may occur in large left to right shunt lesions producing S3.
-
Thus, LV S3 is heard in patients with VSD and PDA, and RV S3 in patients with ASD.
S3 in Mitral Regurgitation
-
It is the result of emptying of large left atrial blood volume into the left ventricle under higher than normal pressure.
-
It is present in any MR that is more than mild.
-
Severe MR is almost always accompanied by S3 (Fig. 5).
-
The presence of S3 in MR does not indicate heart failure.16
-
Absence of S3 in severe MR suggests associated significant mitral stenosis.
-
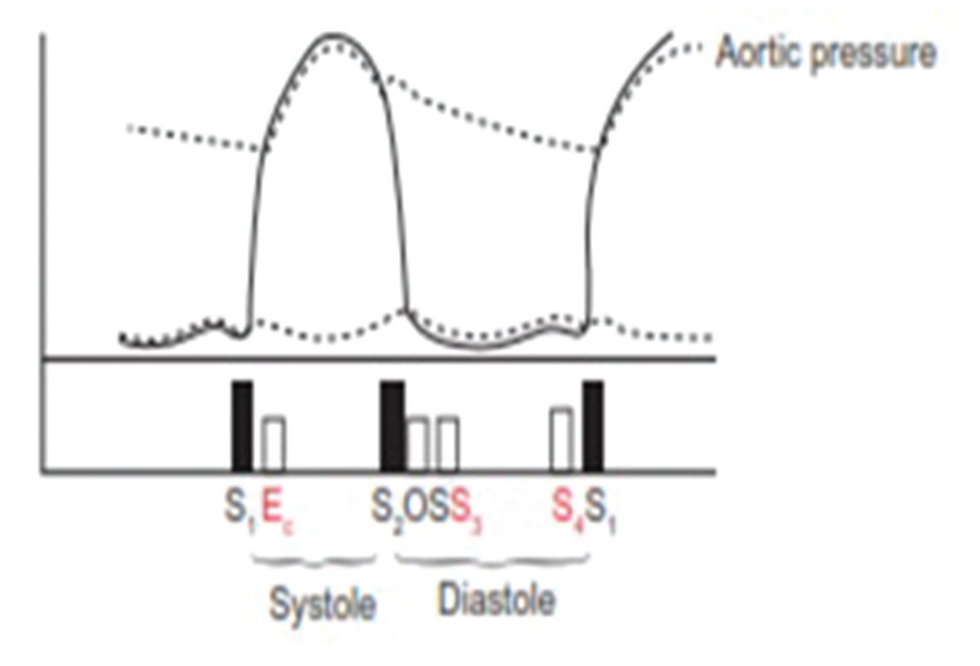
Fig. 5 Mitral phonocardiogram showing pansystolic murmur (SM), opening snap (O), S3 (3) and mid-diastolic rumble (DM) in a patient with severe mitral regurgitation.
Fig. 5 Mitral phonocardiogram showing pansystolic murmur (SM), opening snap (O), S3 (3) and mid-diastolic rumble (DM) in a patient with severe mitral regurgitation.
S3 in Aortic Regurgitation
-
S3 is rarely heard in chronic aortic regurgitation patients.
-
Presence of S3 suggests associated left ventricular dysfunction or MR.
-
AR can produce S3 even in the presence of mitral stenosis because rapid filling can occur through the aortic valve into the left ventricle.
-
In acute AR, S3 may be heard along with diminished or absent S1 in the setting of acute pulmonary edema.17
S3 in Aortic Stenosis
In patients with aortic stenosis, third heart sound is uncommon but it’s presence indicates the presence of systolic dysfunction and elevated filling pressure.18
S3 in Ventricular Systolic Dysfunction
-
Third heart sound is almost always heard in ventricular dysfunction.
-
Presence of S3 usually indicates systolic dysfunction. Various studies have indicated that S3 less sensitive but more specific indicator of decreased ejection fraction (EF).
∘ According to Patel et al, auscultated third and fourth heart sounds are associated with abnormal LV hemodynamics. The sensitivity and specificity for S3 to detect EF < 50% were 51% and 90%, respectively, with a positive predictive value of 95% and a negative predictive value of 32%.
∘ Sensitivity and specificity for detecting EF of < 30% were 78% and 88%, respectively.
∘ The presence of an S3 was also associated with impaired diastolic function as determined by the peak filling rate.19
-
In heart failure patients, S3 gallop is usually associated with the following:
∘ Increased left atrial pressures (>20 mm Hg).
∘ Increased LV end-diastolic pressures (>15 mm Hg).
∘ Elevated serum brain natriuretic peptide (BNP) concentrations.
-
Sensitivity and specificity of S3 to detect elevated BNP levels is approximately 41% and 97%, respectively.20 21
-
S3 may not be heard in mild LV dysfunction.
-
The clinical use of S3 as a sign of heart failure is limited by interobserver variability.22 This can be overcome by using an objective tool to measure heart sounds such as phonocardiography.
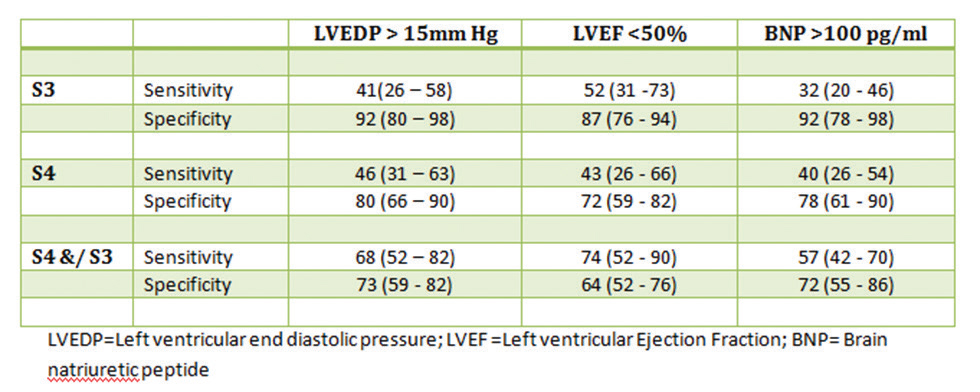
∘ Marcus et al evaluated the diagnostic characteristics of phonocardiographically derived S3 and S4 for detection of LV dysfunction, in patients with heart failure who were undergoing cardiac catheterization.
∘ S3 was not very sensitive (40–50 percent) for the detection of an elevated LV end-diastolic pressure or reduced LVEF.
-
In heart failure patients, S3 is equally prevalent in both symptomatic and asymptomatic LV systolic dysfunction.
-
Thus, presence of S3 in a patient with heart failure suggests ventricular dysfunction as the cause in most of the cases.
-
However, absence of S3 cannot rule out ventricular dysfunction because S3 may be absent in heart failure patients associated with the following:
-
Mitral or tricuspid valve stenosis.
-
Pericardial tamponade.
-
Acute myocardial infarction–S3 may not be heard in early stages of MI. S3 may however occur in later stages due to LV systolic dysfunction or MR.
-
-
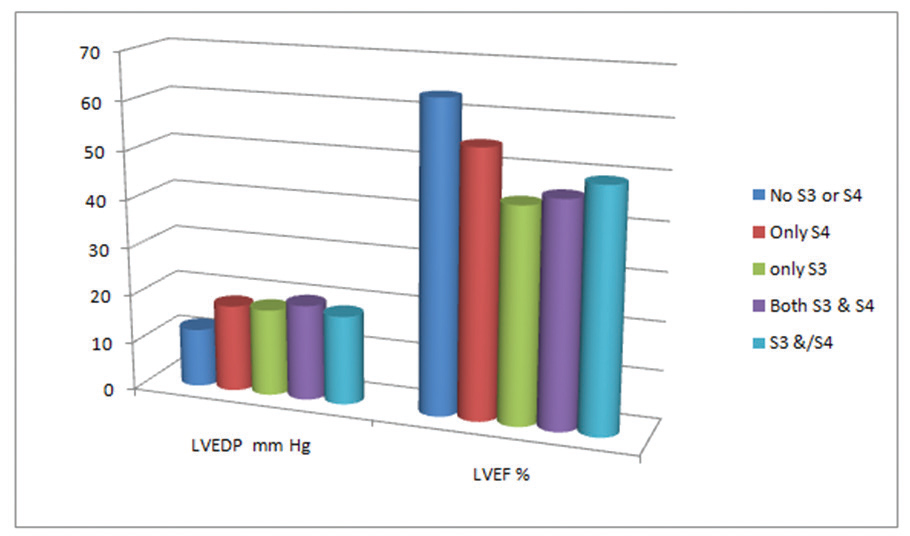
Fig. 6 S3 is more specific but less sensitive marker of elevated LVEDP and decreased EF. (Reproduced with permission from Marcus et al.23). EF, ejection fraction; LVEDP, left ventricular end-diastolic pressure.
Fig. 6 S3 is more specific but less sensitive marker of elevated LVEDP and decreased EF. (Reproduced with permission from Marcus et al.23). EF, ejection fraction; LVEDP, left ventricular end-diastolic pressure.
-
Fig. 7 S3 and or S4 suggest high LVEDP and low LV Ejection Fraction
(Reproduced with permission from Marcus et al.23).
Fig. 7 S3 and or S4 suggest high LVEDP and low LV Ejection Fraction (Reproduced with permission from Marcus et al.23).
The presence of an S3 gallop in heart failure patients also has prognostic significance. In the SOLVD treatment and prevention studies, the investigators found that the presence of S3 is associated with:
-
Higher risk of progression to symptomatic heart failure in asymptomatic LV dysfunction.
-
Higher risk of hospitalization for heart failure (HF) or death from pump failure in patients with overt HF.
-
These observations remained significant even after adjustment for markers of disease severity and were even more powerful when combined with the presence of elevated jugular vein pressure (JVP).24 25
-
In acute myocardial infarction (MI) settings, persistent S3 is associated with increased mortality.
S3 in LV Diastolic Dysfunction
-
S3 is less.. prevalent in diastolic heart failure than systolic heart failure (around 45% in diastolic vs. 65% in systolic HF).26 However, it is difficult to differentiate systolic from diastolic heart failure by clinical signs alone.27
-
Usually, S3 is not heard in patients with impaired relaxation of ventricles. However, rapid early diastolic emptying in the later stages, especially after the onset of systolic dysfunction, may produce a S3 along with S4 (combined systolic and diastolic heart failure).28
Conclusion
Third heart sound (S3) is a low-pitched early diastolic sound, often one of the most difficult sounds to appreciate clinically. Presence of a third heart sound usually signifies either ventricular dysfunction or volume overload of the ventricle. S3 is a useful diagnostic and prognostic finding in patients with either suspected or overt HF. It should be sought out carefully in all patients. Phonocardiogram can be used in difficult cases for the objective assessment of S3.
Fourth Heart Sound (S4)
Definition
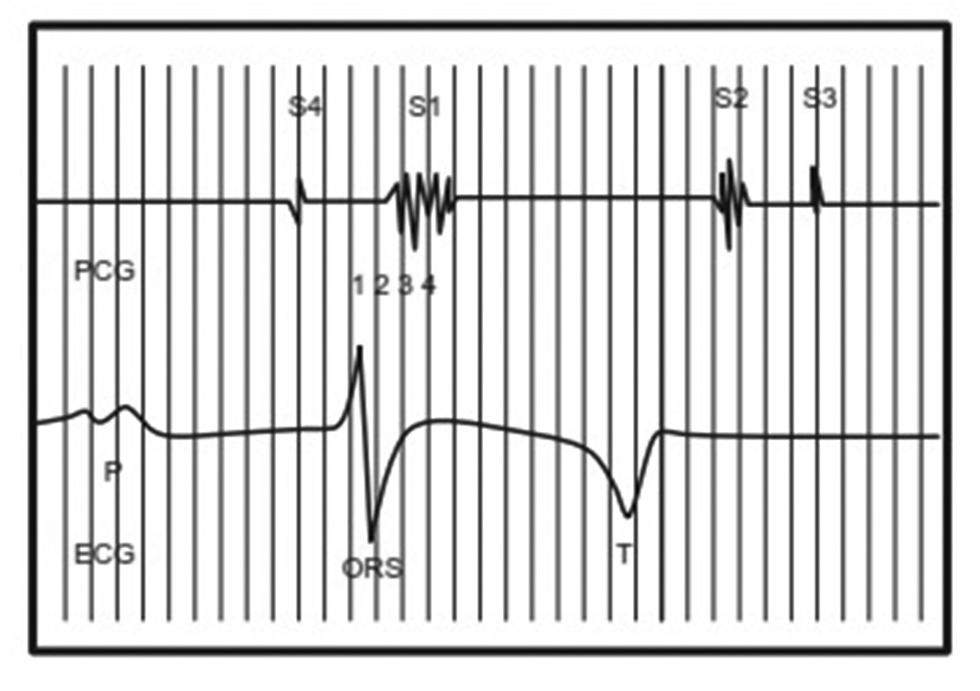
S4 is a low-pitched sound (20–30 Hz) heard in pre systole, that is, shortly before the first heart sound. The rhythm produced by S4 can be compared with the cadence of the word “Tennessee.” The phrase “A-stiff-wall” (a S4, stiff S1, wall S2) can also be used to describe the S4 gallop.29
Synonyms
Atrial gallop and presystolic gallop.
Physiology
Ventricular filling during diastole occurs in two phases. The first, or early rapid filling phase, begins with the opening of the atrioventricular valves and is passive. The second or late rapid filling phase occurs in late ventricular diastole as a result of atrial contraction (Fig. 8). Fourth heart sound is associated with the second active phase of ventricular filling.30
-
Fig. 8 Showing S4 coinciding with the atrial systole.
Fig. 8 Showing S4 coinciding with the atrial systole.
Mechanism
Normally, vibrations generated by atrial contractions are neither audible nor palpable. However, in the presence of a stiff ventricular wall, atrial contractions are more forceful. The sudden deceleration of the inflowing blood following atrial systole generates vibrations in the cardio-hemic system which are heard as S4.31
Increased stiffness of the ventricular wall or decreased compliance of the ventricle is seen in LV hypertrophy or ischemia. In these settings, filling of the nondistensible ventricle results in abnormally increased left ventricular end diastolic pressure (LVEDP), which is seen as a large presystolic “a” wave in the ventricular pressure curve and clinically appreciated as S4 over the precordium.
The exact mechanism of genesis of S4 is not established. The possible theories areas follows:
-
Ventricular theory–Vibrations of the ventricular wall during sudden deceleration of blood flow can produce S4. This theory is no longer accepted.
-
Impact theory–Movement of the ventricle in close proximity to the chest wall after the filling of the ventricle can produces S4.32
Prerequisites for the Genesis of S4
-
Healthy atrium with effective atrial systole.
-
Normal sinus rhythm.
-
Non stenotic AV valve.
-
Noncompliant ventricle.
Clinical Recognition of S4:33 34 35
S4 is a low-frequency sound that is appreciated as a dull sound just before S1. Forceful atrial contractions into a stiff ventricle can produce an early, loud, and palpable S4. S4 may be LV or RV in origin (Table 3).
|
Characteristic feature |
LV S4 |
RV S4 |
|---|---|---|
|
Position |
Left lateral recumbent position |
Supine position |
|
Site of audibility |
Cardiac apex |
Lower left sternal border or subxiphoid region |
|
Respiratory variation |
Better heard in expiration |
Better heard in inspiration |
|
Maneuvers to enhance intensity |
Isometric handgrip |
passive leg |
|
Radiation of sound |
LV S4 may radiate to the brachiocephalic and carotid arteries |
RV S4 may be appreciated over the right internal jugular vein |
|
Other features |
Left-sided causes of S4 |
Prominent ‘a waves’ in JVP |
-
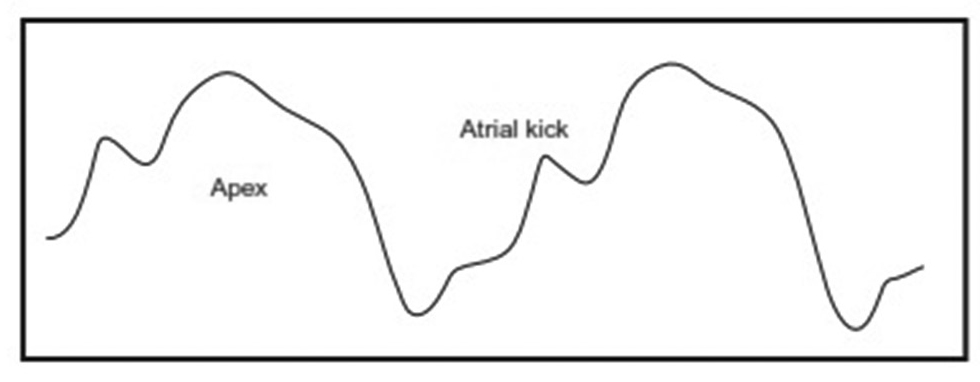
Palpable S4–Audible S4 may be accompanied by a palpable presystolic apical impulse (Fig. 9). Appreciation of a palpable S4 increases the clinical significance of an audible S4.36 Obesity and emphysema may mask a palpable S4. Sometimes, a presystolic outward movement of the cardiac apex may be visible. It can be better appreciated by shining a light tangentially over the cardiac apex or by taping the end of a small stick to the apical area.
-
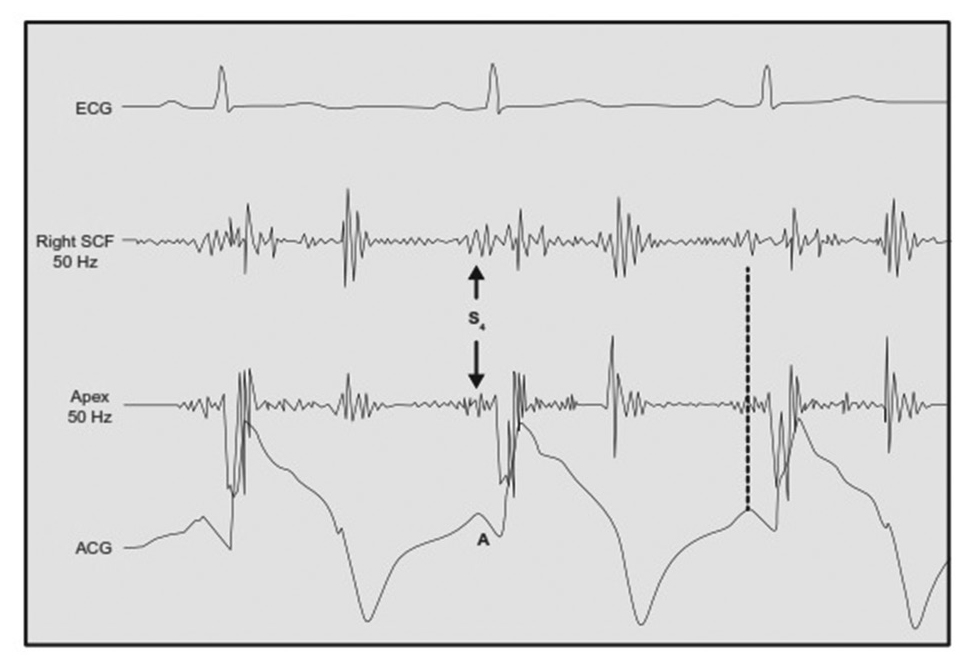
S4 can be appreciated in the apex cardiogram as increased amplitude of the “a” wave (Fig. 10).37 38 39
-
Fig. 9 Case of severe aortic stenosis showing a palpable S4 as “a wave” just before a heaving apical impulse.
Fig. 9 Case of severe aortic stenosis showing a palpable S4 as “a wave” just before a heaving apical impulse.
-
Fig. 10 Case of hypertension showing S4 coincident with the “a” wave of the simultaneously recorded apex cardiogram.
Fig. 10 Case of hypertension showing S4 coincident with the “a” wave of the simultaneously recorded apex cardiogram.
Spodick40 and Adolph41 analyzed the audibility of S4 and came up with the following conclusions:
-
A recordable S4 does not necessarily equate with audibility because most of the filters used in recording systems pass inaudible low-frequency vibrations.
-
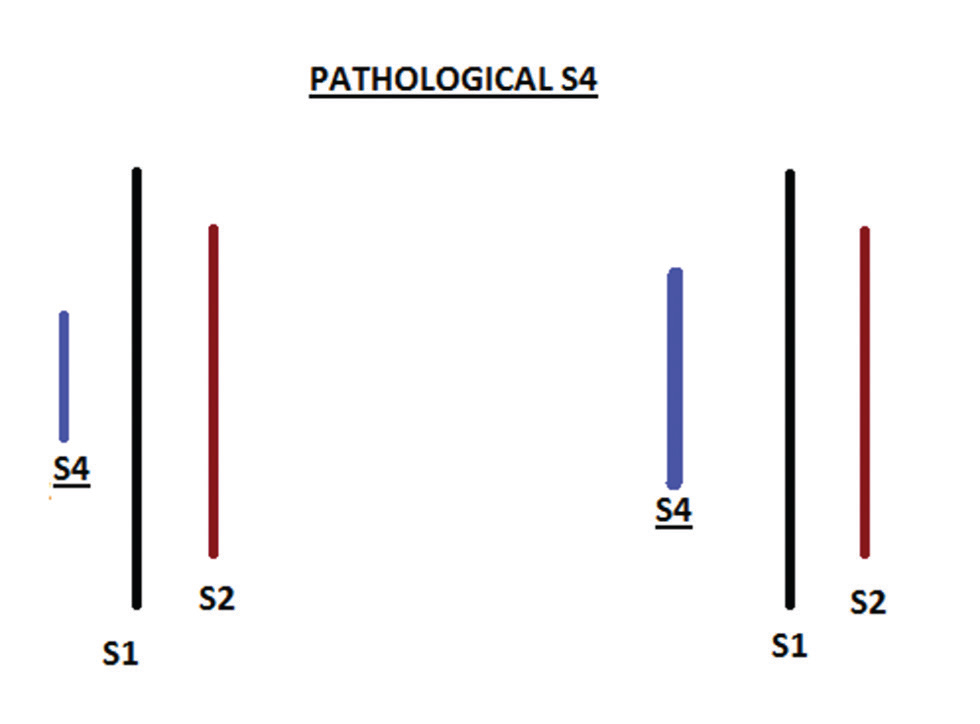
An audible S4 is loud and palpable (Fig. 11).
-
S4 virtually always indicates heart disease.
-
Fig. 11 Pathological S4 is loud and audible.
Fig. 11 Pathological S4 is loud and audible.
S4–S1 Interval
-
S4 coincides with atrial contraction and occurs 70 milliseconds after the P wave in ECG.
-
Audibility of S4 not only depends on its intensity and frequency but also on its separation from S1, which is referred to as the S4–S1 interval.
-
This interval may be influenced by PR interval, P–S4 interval, and Q–S1 interval.
-
In conditions where PR interval is prolonged, as in first degree heart block, there is increase in S4–S1 interval. This enables better appreciation of S4.
-
In patients with tachycardia, where PR interval is short, it is difficult to appreciate S4.
-
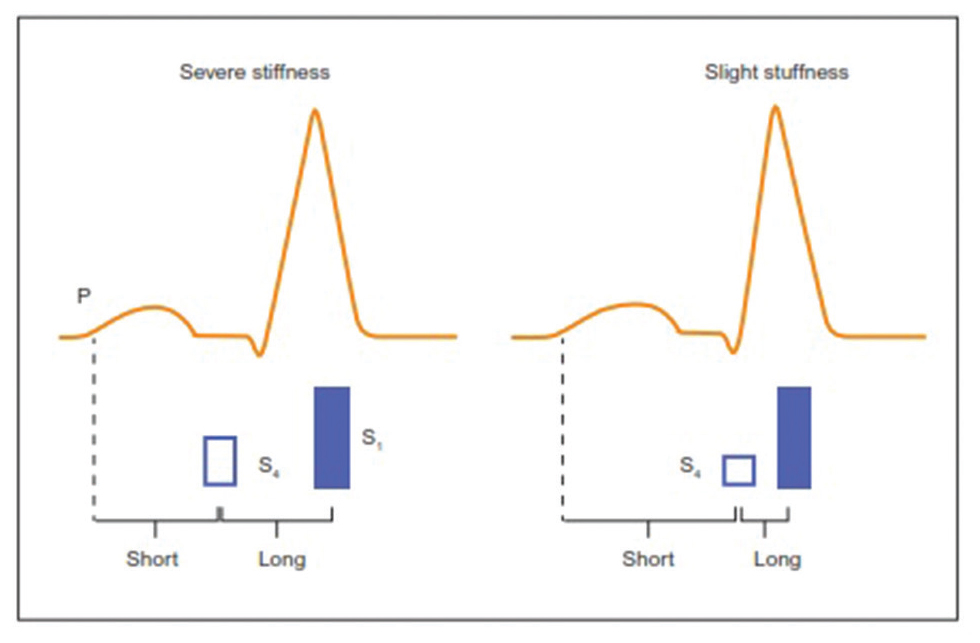
Increase in ventricular stiffness is associated with a loud and earlier S4, with increase in the S4–S1 interval (Fig. 12).
-
In heart failure patients, longer interval between S4 and S1 represents exacerbation of heart failure.42 and poor prognosis.43
-
Fig. 12 Increase in ventricular stiffness is associated with increase in the S4–S1 interval.
Fig. 12 Increase in ventricular stiffness is associated with increase in the S4–S1 interval.
Differential Diagnosis
-
Split S1–Higher in frequency, more widely heard over the precordium, and no postural variations.
-
S3.
-
Opening snap of MS.
-
Pericardial knock of constrictive pericarditis.
-
Tumor plop of atrial myxoma.
-
Prosthetic valve sounds.
Absent S4
-
Sinus rhythm–S4 is not audible in AF or flutter.
-
Shortened PR interval–In patients with tachycardia, it is difficult to appreciate S4.
-
Severe MS or tricuspid stenosis.
-
If EDP is very high, that is, >25 mm Hg, S4 may be absent because of insufficient pumping function of atria
-
Obesity and emphysema.
S4 and Atrial Fibrillation
In patients with noncompliant ventricles, there is restriction of early filling and increased dependency on ventricular filling due to atrial contraction. However, in atrial fibrillation (AF), loss of effective atrial kick impairs ventricular filling, elevating the LV end diastolic volume and LVEDP, leading to heart failure.
-
Clinically, S4 is not heard when patient develops AF.
-
However, multiple, irregular medium- to high-pitched clicking sounds may be heard at the base or midparasternal areas.
-
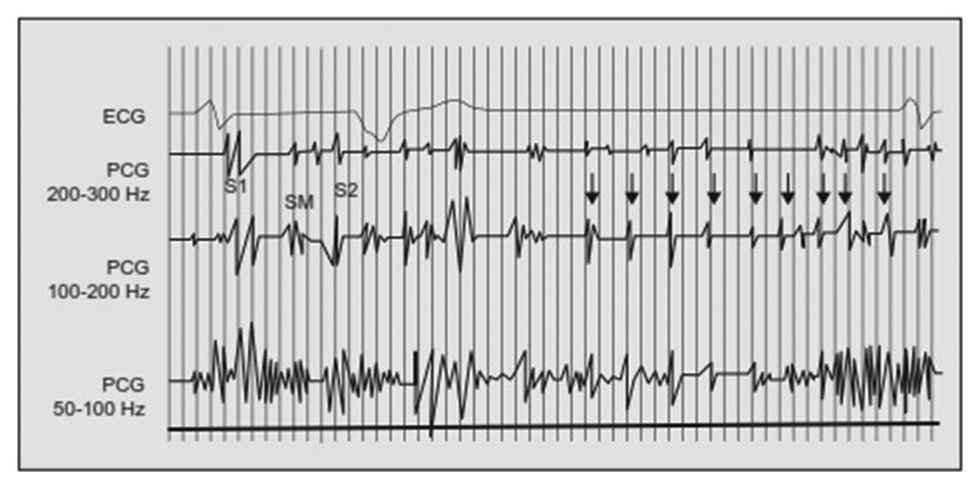
These sounds are heard in both systole and diastole at a rate of approximately 480/min and correspond to the fibrillation or f waves in ECG (Fig. 13).
-
The these atrial.. sounds are believed to arise from the forceful atrial contractions that are transmitted to mitral valve, aortic valves, and other intracardiac structures.
-
They are more commonly heard in patients with congestive heart failure and coarse AF or flutter and slow ventricular rate with long diastolic pauses.
-
They tend to disappear with improvement of HF or increase in heart rate.44 45
-
Fig. 13 Phonocardiogram showing multiple, irregular, medium frequency atrial sounds (arrows) in a patient with coarse atrial fibrillation.
Fig. 13 Phonocardiogram showing multiple, irregular, medium frequency atrial sounds (arrows) in a patient with coarse atrial fibrillation.
Causes
S4 can be of either right or left ventricular in origin (Fig. 14).
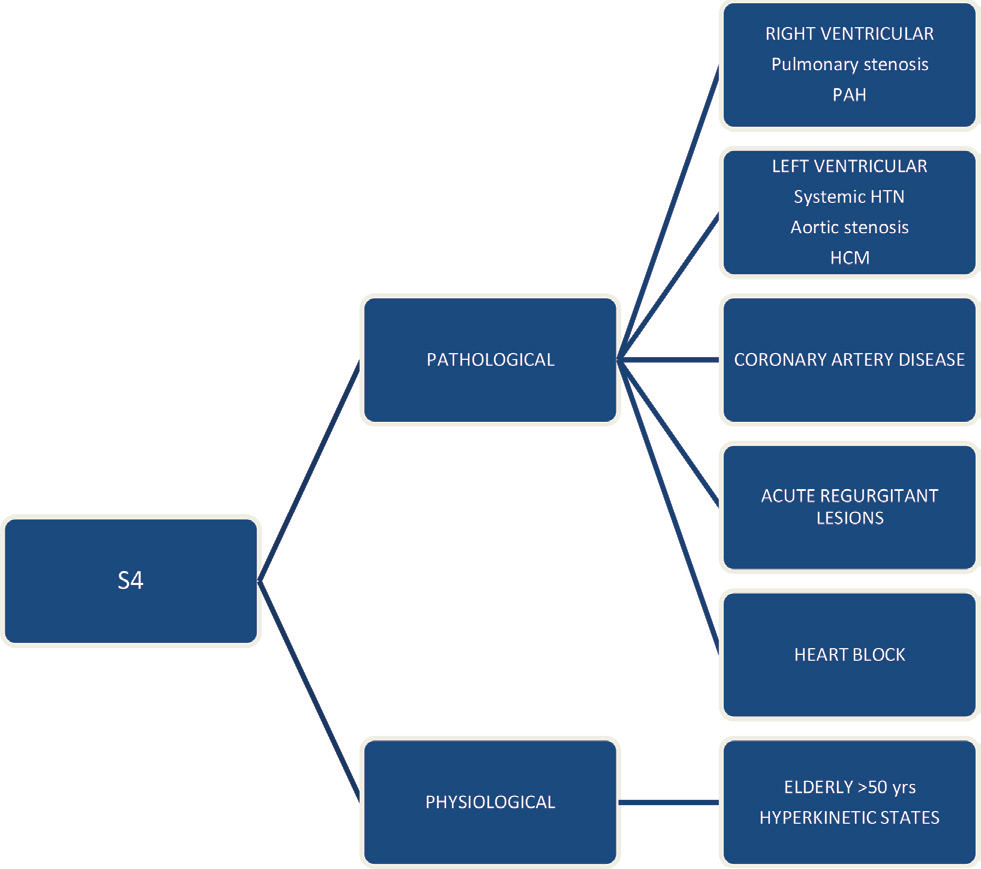
-
Fig. 14 Causes of S4.
Fig. 14 Causes of S4.
Clinical Significance of S4
-
S4 is an indirect sign of increased stiffness of the ventricular wall.
-
It is associated with conditions pertaining to decreased ventricular compliance such as LV hypertrophy.
-
Presence of S4 usually signifies an abnormally increased ventricular end-diastolic pressure (RVEDP > 12 mm Hg and LVEDP of > 15 mm Hg).
S4 and Age
S4 is usually heard in those > 50 years of age and is attributed to decreased ventricular compliance with advanced age. Prevalence of S4 in elderly is highly variable with a prevalence of 11 to 75%, according to various phonocardiography studies.
-
In a study by Collins et al:
∘ Prevalence of S4 in asymptomatic adults (18–94 years) was 15.6% (95% Cl, 13.2–18.2%).
∘ Prevalence of S3 was 10% (95% CI,8.1–12.2%).
∘ Prevalence of both S3 and S4 were 3.5% (95% Cl, 2.4–5.0%).
∘ Increasing age was found to decrease the odds of an audible S3 (odds ratio, 0.96; 95% Cl, 0.95–0.96) and increase the odds of an audible S4 (odds ratio, 1.04; 95% Cl, 1.03–1.05).46
-
Spodick and Quarry had examined 250 consecutive ambulatory subjects in the Framingham Heart Study and found a phonocardiographic S4 to be present in 73.1% of healthy patients and 74.3% of patients with cardiovascular (CV) disease.
∘ A study of 100 patients (50% healthy and 50% hypertensive)–a 70% prevalence of S4 was seen in both.47
∘ Eriksen et al studied the presence of S4 by phonocardiography and auscultation prospectively in 1714 healthy men (40–59 years). S4 was associated with higher blood pressure, coronary artery disease and its risk factors but not with age. They concluded that S4 is probably not a completely innocent finding.48
Thus, detection of S4, even in the elderly, should not be ignored. When S4 is loud and palpable, regardless of age, it is almost always pathological. Hypertension and coronary artery disease are the most common associated lesions.
S4 in Hyperkinetic States
-
In hyperkinetic states like anemia, thyrotoxicosis, etc., vigorous atrial contractions into a volume overloaded, noncompliant ventricle may produce a S4.
-
Accompanying tachycardia may fuse S3 with S4 to produce a diastolic rumble or a loud summation gallop.
S4 in Hypertension
-
LV hypertrophy associated with increased afterload due to systemic hypertension decreases the compliance of the ventricles and produces a S4.
-
However, when flash pulmonary edema occurs due to hypertension, S3 is more common than S4. Transient systolic dysfunction, transient diastolic regurgitation, or MR are the probable underlying mechanisms.
S4 in LV Outflow Obstruction
-
In patients with aortic stenosis, presence of S4 suggests at least moderate degree of obstruction.49
-
When there is accompanying severe mitral stenosis (MS) or AF, S4 may be absent.
-
Associated coronary artery disease (CAD) may also produce a S4 in patients with mild-to-moderate aortic stenosis.
Caulifield et al studied the significance of S4 in clinical assessment of severity in 124 patients with discrete obstruction to LV outflow. The results indicate the following
-
In patients > 40 years age, S4 is not a reliable index of severity in discrete aortic stenosis.
-
In patients < 40 years age, S4 suggests a peak systolic gradient of 75 mm Hg or more.
-
Absence of S4 in any adult suggests that the peak gradient is less than 75 mm Hg and probably less than 60 mm Hg, provided that factors hindering detection of a fourth heart sound (such as very short P-R interval, emphysema or obesity) are taken into account.50
-
In patients with hypertrophic cardiomyopathy (HCM), S4 is consistently present irrespective of the degree of obstruction. Therefore, S4 cannot be correlated with severity of left ventricular outflow tract (LVOT) obstruction.51
S4 in Acute Regurgitant Lesions
-
MR–In chronic MR, presence of dilated LV preludes the occurrence of S4.
-
However, S4 may be heard in MR in the following conditions:
-
Acute MR
-
Hypertensive patients
-
Associated CAD
-
S4 in a patient with MR suggests elevated LVEDP, especially when associated with S3.52 53
-
Aortic regurgitation (AR)–S4 is heard when AR is acute in onset. In chronic AR with decreased LV compliance due to associated lesions (e.g., systemic hypertension or CAD), S4 may occur.
S4 in Myocardial Disease
S4 is commonly heard when there is reduced LV compliance associated with acute myocarditis and restrictive cardiomyopathies, as in endomyocardial fibroelastosis.
S4 in Coronary Artery Disease
S4 is commonly heard during the early stages of acute MI. It can occur with or without signs of heart failure. It does not per se indicate LV dysfunction.
-
Hill et al evaluated the diagnostic value of S4 in consecutive MI patients.
∘ Most patients with acute infarction had atrial gallops.
∘ S4 was absent in one patient with preexisting MS and another with left atrial fibrosis on postmortem examination.
∘ They suggested that the absence of an atrial gallop in a patient presenting with chest pain and in sinus rhythm makes the diagnosis of MI less likely.54
S4 may become evident, or its intensity may be augmented, during episodes of angina pectoris.55 Audible and/or palpable atrial gallops are a frequent finding in chronic LV aneurysm and are usually associated with LV dyskinesia.
S4 in LV Dysfunction
-
Presence of S4 in a patient with LV dysfunction suggests underlying decreased ventricular compliance.
-
The sensitivity of S4 to detect an elevated LVEDP, reduced LVEF, or elevated BNP is 46%, 43%, and 40%, respectively, and specificity is 80%, 72%, and 78%, respectively.56
-
S4–S1 interval is a useful index in patients with heart failure. The interval is prolonged by exacerbation and shortened by improvement of HF.
∘ In a study by Tabuchi et al, the S4–S1 interval was 102 ± 24 milliseconds during exacerbation of HF and shortened to 76 ± 18 milliseconds after improvement of HF.42
-
Meyers et al studied the correlation of S4 with level of severity of LV diastolic dysfunction. S4 was audible in 35% with normal function, 42% with mild, 70% with moderate, and none with severe dysfunction (p = 0.052).
∘ Sensitivity was 43%, specificity 65%, and accuracy 53% for discriminating normal from abnormal function.
∘ They concluded that S4 is not a useful indicator of severity of LV diastolic dysfunction.57
S4 in Heart Block
-
Prolonged PR interval in first degree AV block facilitates audibility of S4, as S4–S1 interval is increased (Fig. 15).
-
In second degree AV block, isolated S4 may be heard.
-
In complete heart block multiple, independent S4 sounds are heard at a rate faster than the ventricular escape rate.58
-
Fig. 15 First degree heart block with increased S4–S1 interval.
Fig. 15 First degree heart block with increased S4–S1 interval.
Right Ventricular S4
RV S4 is heard in RV outflow tract (RVOT) obstruction. It can also be heard in pulmonary arterial hypertension and acute pulmonary thromboembolism, provided there is no atrial fibrillation. RV S4 usually indicates right ventricular pressures are in the systemic range. It is usually associated with a prominent “a” wave in JVP.
-
In patients with RVOT obstruction, RV S4 suggests there is, at least, moderate degree of obstruction.
-
In patients with pulmonary stenosis, RV S4 suggests intact atrial and ventricular septum. If there is an associated ASD or VSD, S4 will not be heard.
Conclusion
S4 or atrial gallop is a low-pitched diastolic sound heard just before S1. When S4 is loud and palpable, it is always pathological and indicates decreased compliance of the ventricles. In a patient with chest pain, presence of S4 usually indicates myocardial ischemia as the cause, provided the patient is in sinus rhythm. In patients with heart failure, S4–S1 interval is useful in early detection of exacerbations and may emerge as a useful prognostic tool in the future.
Conflict of Interest
None.
References
- Investigation of genesis of gallop sounds in dogs by quantitative phonocardiography and digital frequency analysis. Circulation. 1985;71(05):987-993.
- [Google Scholar]
- Relationship of the third heart sound to transmitral flow velocity deceleration. Circulation. 1995;92(03):388-394.
- [Google Scholar]
- The Normal Third Heart Sound and Gallops.Hurst, The Heart. (5th ed). New York: McGraw-Hill; 1982. p. :224-31. In:
- [Google Scholar]
- The genesis of gallop sounds investigation by quantitative phono and apex cardiography. Circulation. 1983;63:992-933.
- [Google Scholar]
- Normal and abnormal heart sounds in cardiac diagnosis: Part II. Diastolic sounds. Curr Probl Cardiol. 1985;10(04):1-55.
- [Google Scholar]
- Craige Localization of the origin of the third heart sound. Circulation. 1982;66:II210.
- [Google Scholar]
- Origin of the third heart sound. II. Studies in human subjects. Circulation. 1983;67(02):399-404.
- [Google Scholar]
- Third Heart Sound and Summation Gallop Physiologic Principles of Heart Sounds and Murmurs. New York: American Heart Association; 1975. p. :79-84.
- [Google Scholar]
- Chapter 24 The Third Heart Sound. In: Clinical Methods: The History, Physical, and Laboratory Examinations 3rd edition. Boston: Butterworths; 1990.
- [Google Scholar]
- Current concepts of the genesis of heart sounds. II. Third and fourth sounds. JAMA. 1978;239(26):2790-2791.
- [Google Scholar]
- The mechanism of disappearance of the physiologic third heart sound with age. Circulation. 1986;73(05):877-884.
- [Google Scholar]
- The noninvasive cardiac evaluation of long-distance runners. Chest. 1978;73(03):376-381.
- [Google Scholar]
- Clinical significance and hemodynamic correlates of the third heart sound gallop in aortic regurgitation. A guide to optimal timing of cardiac catheterization. Circulation. 1981;64(03):464-471.
- [Google Scholar]
- Implications of third heart sounds in patients with valvular heart disease. N Engl. J Med. 1992;327:458-462.
- [Google Scholar]
- Implications of an audible third heart sound in evaluating cardiac function. West J Med. 1993;158(06):606-609.
- [Google Scholar]
- Echocardiographic, neurohormonal and invasively measured correlates of third and fourth heart sounds determined by audioelectriccardiography. J Am Soc Echocardiogr. 2004;17:523.
- [Google Scholar]
- Usefulness of the third heart sound in predicting an elevated level of B-type natriuretic peptide. Am J Cardiol. 2004;93(10):1312-1313.
- [Google Scholar]
- Interobserver agreement by auscultation in the presence of a third heart sound in patients with congestive heart failure. Chest. 1987;91(06):870-873.
- [Google Scholar]
- Association between phonocardiographic third and fourth heart sounds and objective measures of left ventricular function. JAMA. 2005;293(18):2238-2244.
- [Google Scholar]
- Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med. 2001;345(08):574-581.
- [Google Scholar]
- Third heart sound and elevated jugular venous pressure as markers of the subsequent development of heart failure in patients with asymptomatic left ventricular dysfunction. Am J Med. 2003;114(06):431-437.
- [Google Scholar]
- Hospitalized congestive heart failure patients with preserved versus abnormal left ventricular systolic function: clinical characteristics and drug therapy. Am J Med. 1995;99(06):629-635.
- [Google Scholar]
- Utility of history, physical examination, electrocardiogram, and chest radiograph for differentiating normal from decreased systolic function in patients with heart failure. Am J Med. 2002;112(06):437-445.
- [Google Scholar]
- New concepts in diastolic dysfunction and diastolic heart failure: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation. 2002;105(11):1387-1393.
- [Google Scholar]
- Textbook of Physical Diagnosis History and Examination. (7th edition). 1989. Reprinted 2014
- [Google Scholar]
- The fourth heart sound.Physiologic Principles of Heart Sounds and Murmurs. New York: American Heart Association; 1975. p. :74-78. In: eds.
- [Google Scholar]
- Relationship of the fourth heart sound to atrial systolic transmitral flow deceleration. Am J Physiol. 1997;272:H1527-H1536. (3 Pt 2)
- [Google Scholar]
- The genesis of the third and fourth heart sounds. A pressure-flow study in dogs. J Clin Invest. 1984;73(05):1400-1407.
- [Google Scholar]
- Eric S. Williams. Chapter 25 The Fourth Heart Sound Clinical Methods: The History, Physical, and Laboratory Examinations 3rd edition. Boston: Butterworths; 1990
- Auscultatory perception of the fourth heart sound: effects of interval form fourth to first sound (S4-S1) and aging. Am J Cardiol. 1976;37(06):848-852.
- [Google Scholar]
- Concerning the cardiac rhythm called gallop rhythm.Classic Descriptions of Disease. Springfield: Charles C Thomas; 1965. p. :388-90. In: ed.
- [Google Scholar]
- The Cause and Clinical Significance of Diastolic Heart Sounds. Arch Intern Med. 1980;140(04):537-541.
- [Google Scholar]
- Audibility of the fourth heart sound. Relationship to presence of disease and examiner experience. Arch Intern Med. 1987;147(04):721-726.
- [Google Scholar]
- Audibility of the fourth heart sound. A prospective, “blind” auscultatory and polygraphic investigation. JAMA. 1972;221(01):36-41.
- [Google Scholar]
- The clinical value of the calibrated apical A wave and its relationship to the fourth heart sound. Circulation. 1979;60(06):1412-1421.
- [Google Scholar]
- [Mechanism and clinical usefulness of S4-S1 interval in heart failure associated with left ventricular inflow pattern] J Cardiol. 1998;31(05):273-279.
- [Google Scholar]
- Yaeger K, Norton M, Jala S. The S4 Gallop.Learning Cardiac Auscultation From Essentials to Expert Clinical Interpretation 2015
- Mechanism of atrial sounds in atrial fibrillation. Phonoechocardiographic correlation. Report of a case. Circulation. 1976;53(03):569-571.
- [Google Scholar]
- Prevalence of the Third and Fourth Heart Sound in Asymptomatic Adults. Congestive heart failure. 2005;11:242-247.
- [Google Scholar]
- Prevalence of the fourth heart sound by phonocardiography in the absence of cardiac disease. Am Heart J. 1974;87(01):11-14.
- [Google Scholar]
- Prevalence and significance of the fourth heart sound (S4) in presumably healthy middle-aged men, with particular relation to latent coronary heart disease. Eur J Cardiol. 1979;9(01):63-75.
- [Google Scholar]
- Hemodynamic-phonocardiographic correlations of the fourth heart sound in aortic stenosis. Circulation. 1962;26:92-98.
- [Google Scholar]
- Walter H. Caulfield, MD, Antonio C. deLeon Jr., MD, FACC, Joseph K. Perloff, MD, FACC, R. Barrett Steelman, MD. The clinical significance of the fourth heart sound in aortic stenosis. Symposium on cardiovascular sound volume. Issue 2. P179–18. August 01, 1971
- Idiopathic hypertrophic subaortic stenosis: clinical, hemodynamic and angiographic manifestations. Am J Med. 1960;29:924-945.
- [Google Scholar]
- Diagnosis of severe mitral regurgitation due to non-rheumatic chordal abnormalities. Br Heart J. 1973;35(09):877-886.
- [Google Scholar]
- Echocardiographic, neurohormonal and invasively measured correlates of third and fourth heart sounds determined by audioelectric cardiography. Am Soc Echocardiogr. 2004;17:52.
- [Google Scholar]
- The diagnostic value of the atrial gallop in acute myocardial infarction. Am Heart J. 1969;78(02):194-201.
- [Google Scholar]
- Resting and postexercise phonocardiogram and electrocardiogram in patients with angina pectoris and in normal subjects. Circulation. 1971;43(02):273-277.
- [Google Scholar]
- Association between phonocardiographic third and fourth heart sounds and objective measures of left ventricular function. JAMA. 2005;293(18):2238-2244.
- [Google Scholar]
- Correlation of an audible fourth heart sound with level of diastolic dysfunction. Am J Med Sci. 2009;337(03):165-168.
- [Google Scholar]
- Stephen M. Reed, Warwick M. Bayly, Debra C. Sellon. Equine Internal Medicine.Disorders of Cardiovascular System. 4th edition 2018.







