Translate this page into:
Acute Anterior Wall Myocardial Infarction in a Gallbladder Cancer Patient: A Case of Sudden Coronary Thrombosis Post-normal Angiogram
*Corresponding author: Akif Ahamad Baig, Department of Cardiology, Aster Ramesh Hospital, Guntur, Andhra Pradesh, India. akifab93@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Baig AA, Sandeep J, Mahathi T, Haritha N. Acute Anterior Wall Myocardial Infarction in a Gallbladder Cancer Patient: A Case of Sudden Coronary Thrombosis Post-Normal Angiogram. Indian J Cardiovasc Dis Women. 2024;9:246-8. doi: 10.25259/IJCDW_42_2024
Abstract
Cancer patients face a heightened risk for thromboembolic events, including arterial thromboembolism such as myocardial infarction (MI). Thrombosis is a major cause of mortality in these patients due to the hypercoagulable state induced by malignancy and its treatments. Pro-inflammatory cytokines and pro-coagulants secreted by tumor cells lead to endothelial damage and an increased risk of thrombus formation. Despite extensive research on venous thromboembolism in cancer, arterial thromboembolism remains less studied. This case report highlights an acute anterior wall MI in a patient with metastatic gallbladder cancer, who developed a sudden thrombotic event despite having a normal coronary angiogram shortly before. A 52-year-old female with metastatic gallbladder cancer presented to the emergency department with acute chest pain. Her cancer, diagnosed 6 months earlier, had been managed with cholecystectomy and subsequent chemotherapy. Fifteen days before her current admission, she had undergone a coronary angiogram due to atypical chest pain, which showed no significant coronary artery disease. At presentation, the patient reported, sudden chest pain radiating to the left arm. She was hemodynamically stable with normal blood pressure and heart rate. The physical examination was unremarkable. Electrocardiogram segment elevation (ST)-segment elevation in anterior leads (V2-V6) and limb leads (II, II, and augmented vector foot [aVF]), indicative of an acute anterior wall MI. Elevated cardiac biomarkers confirmed myocardial injury. A two-dimensional echocardiogram showed mild hypokinesia of the distal interventricular septum and the apex. A repeat coronary angiogram identified a thrombus in the left anterior descending artery, which was not present in the previous angiogram. The rapid appearance of the thrombus pointed to an acute thrombotic event. This case illustrates the aggressive nature of thrombotic events in cancer patients. Despite a normal angiogram 2 weeks prior, the patient developed a sudden coronary thrombus, reflecting the hypercoagulable state associated with malignancy. The management involved thrombus aspiration and tirofiban, which effectively resolved the acute event. This aligns with existing literature, emphasizing the need for vigilant monitoring and proactive management in cancer patients to address the risk of rapid-onset thrombotic events. Cancer patients can experience sudden and severe thrombotic events, even with recent normal coronary evaluations. This case highlights the importance of ongoing cardiovascular assessment and tailored therapeutic strategies in managing cancer-associated thrombosis, underscoring the need for a collaborative approach between oncologists and cardiologists.
Keywords
malignancy
myocardial infarction
coronary angiogram
coronary thrombosis
acute coronary syndrome
INTRODUCTION
Malignancy is a significant risk factor for thromboembolic events, including both venous and arterial types such as myocardial infarction (MI). Thrombosis is notably the second most common cause of death in cancer patients, primarily due to the hypercoagulable state induced by the malignancy and its treatments. This state is driven by several mechanisms: the secretion of pro-inflammatory cytokines and pro-coagulants from tumor cells, leading to endothelial damage, increased vascular permeability, decreased levels of coagulation inhibitors, and impaired fibrinolysis. These factors collectively enhance the risk of thrombotic events.[1,2]
While much research has focused on venous thromboembolism in cancer patients, there is limited information on arterial thromboembolism. This gap is particularly concerning as cancer patients can rapidly develop acute coronary syndromes despite having a normal coronary angiogram. This case report highlights the complexities involved in managing such patients by detailing a 52-year-old female with metastatic gallbladder cancer who suffered an acute anterior wall MI despite having a normal angiogram just weeks prior.
CASE REPORT
A 52-year-old woman, non-diabetic, non-hypertensive, was diagnosed with metastatic gallbladder cancer 6 months prior and receiving chemotherapy and radiation therapy. Fifteen days before her current presentation, she had a coronary angiogram due to atypical chest pain, which showed no significant coronary artery disease. She presented to the emergency department with sudden chest pain radiating to her left arm, accompanied by sweating. On arrival, she was hemodynamically stable with normal blood pressure and heart rate. Physical examination did not reveal any significant abnormalities.
An electrocardiogram showed ST-segment elevation in the anterior leads (V2-V6) and limb leads (II, II, and aVF) [Figure 1], indicating an acute anteroinferior wall MI. A 2D echocardiogram revealed mild hypokinesia of the distal interventricular septum and the apex.
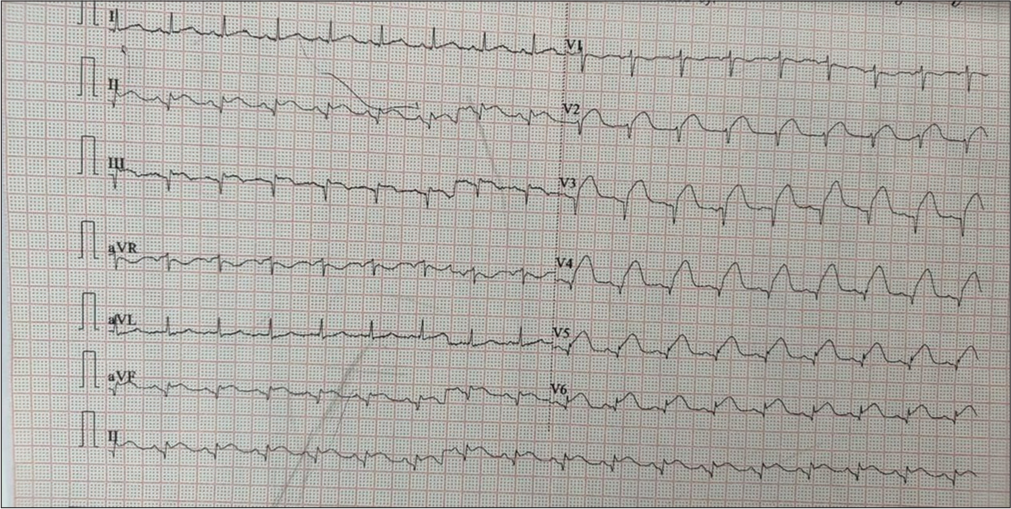
- 12 Lead standard electrocardiogram showing ST segment elevation in leads V2-V6, lead II, III, and aVF. Leads V2-V6 represent the precordial (chest) leads on an electrocardiogram (ECG), which monitor electrical activity in the anterior and lateral regions of the heart. (ST: segment elevation, aVF: augmented vector foot.)
A repeat coronary angiogram was performed, which revealed a thrombus in the left anterior descending artery [Figure 2], a finding that was not present in the angiogram performed 15 days earlier [Figure 3].
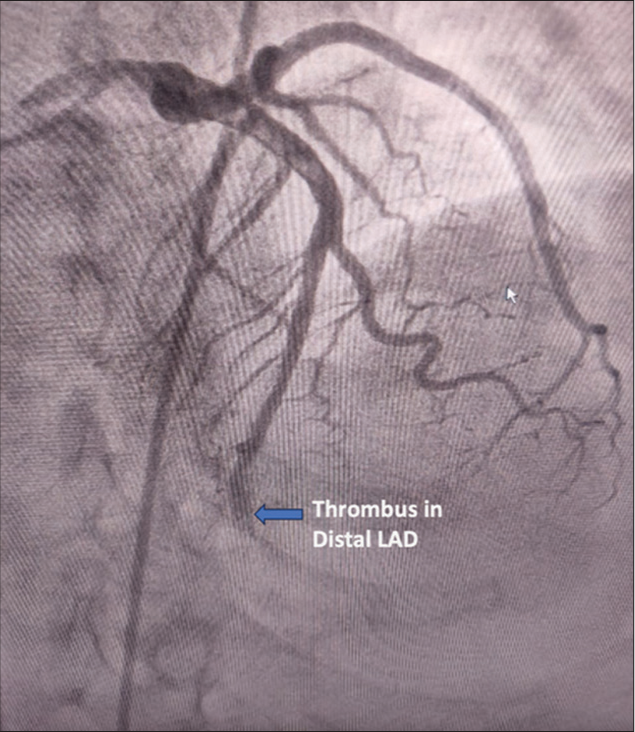
- Coronary angiogram showing thrombotic occlusion in distal left anterior descending artery. The blue arrow indicates the location of the thrombotic occlusion in the distal left anterior descending artery. (LAD: Left anterior descending artery).
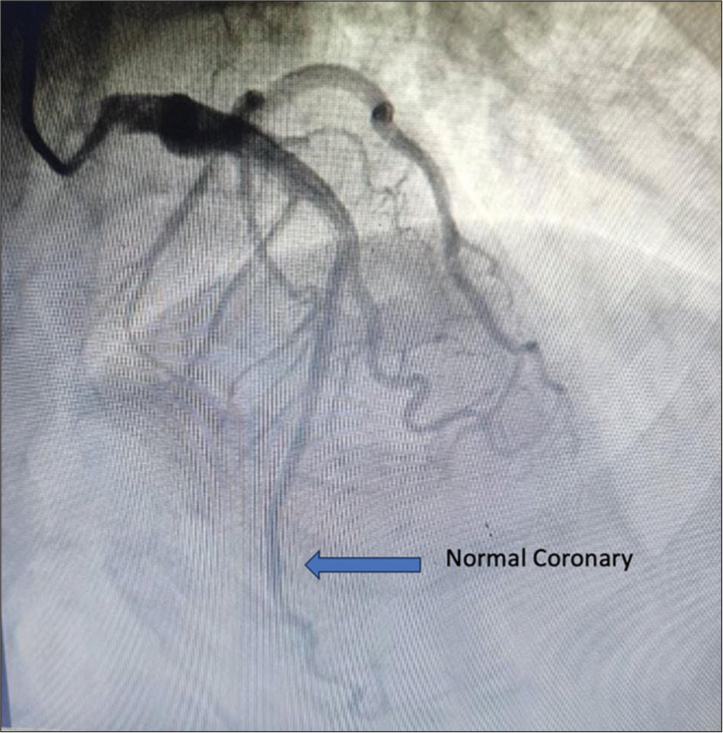
- Coronary angiogram performed 15 days prior showing normal flow in distal left anterior descending artery. The blue arrow highlights the normal flow in the distal left anterior descending artery in the angiogram performed 15 days earlier.
The patient was treated with thrombus aspiration and intracoronary tirofiban followed by an intravenous tirofiban infusion. Antiplatelets, statins, and anticoagulation were given. After the procedure, she was monitored in the coronary care unit and gradually improved.
DISCUSSION
Cancer is a well-established risk factor for thromboembolic events, including both venous and arterial types. Thrombosis, particularly arterial thromboembolism, represents a major concern in cancer patients due to the hypercoagulable state associated with malignancy. This state is mediated by various factors including the secretion of pro-inflammatory cytokines and pro-coagulants from neoplastic cells, which induce endothelial damage, increase vascular permeability to platelet-activating factors, and decrease levels of anticoagulants. These changes create an environment conducive to thrombus formation.
The rapid onset of coronary thrombosis in our patient, despite having a normal angiogram just weeks earlier, underscores the aggressive nature of cancer-related thrombotic events. The previous studies, such as those by Navi et al.,[1] have documented an increased incidence of arterial thromboembolism in cancer patients, highlighting the need for heightened vigilance and proactive management strategies. This case is consistent with these findings, demonstrating how cancer can precipitate acute coronary events even in the absence of detectable atherosclerosis.
The study by Mahajan et al.[2] similarly describes a case where a patient with metastatic cancer developed acute coronary syndrome despite a recent normal angiogram. This comparison emphasizes the unpredictable nature of cancer-associated thrombotic events and the importance of aggressive management strategies. Both cases involved thrombus aspiration and antithrombotic therapy, reflecting a common approach in managing such acute events in cancer patients.
Further supporting this view, Zhang et al.[3] highlighted the increased risk of arterial thrombosis in cancer patients and stressed the importance of thorough cardiovascular risk assessment and management. The study found that cancer patients often have elevated levels of pro-coagulant factors, which align with our case where the patient developed a thrombus rapidly due to the hypercoagulable state induced by cancer and its treatments.
In addition, Li et al.[4] provided insights into the mechanisms underlying cancer-associated arterial thrombosis, showing that elevated circulating tissue factor levels contribute significantly to thrombotic risk. This aligns with our case, where the aggressive nature of the thrombus and its sudden appearance can be attributed to the elevated pro-coagulant state.
The treatment approach in our case, involving thrombus aspiration and tirofiban administration, is consistent with recommendations for managing acute coronary syndromes in patients without significant atherosclerosis. This approach is supported by prior literature, including the study by Mantha et al.,[5] which emphasized the effectiveness of anticoagulation and antiplatelet therapy in similar scenarios.
CONCLUSION
Acute MI can occur unexpectedly in cancer patients, even with recent normal coronary angiograms. Close collaboration between oncologists and cardiologists is essential in managing these patients, considering the prothrombotic risks associated with cancer and its treatments.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Risk of Arterial Thromboembolism in Cancer Patients: A Systematic Review and Meta-analysis. J Am Heart Assoc. 2017;6:e007953.
- [Google Scholar]
- Myocardial Infarction in Cancer Patients: A Case Report and Review of the Literature. Cureus. 2021;13:e12507.
- [Google Scholar]
- The Risk of Arterial Thrombosis in Cancer Patients: A Comprehensive Review. J Clin Med. 2022;11:1792.
- [Google Scholar]
- Mechanisms of Cancer-Associated Arterial Thrombosis: A Review. Cancers. 2023;16:2238.
- [CrossRef] [PubMed] [Google Scholar]
- Anticoagulation and Antiplatelet Therapy in Cancer-Associated Myocardial Infarction. J Thromb Thrombolysis. 2017;44:493-500.
- [Google Scholar]







