Translate this page into:
A Study of Fertility and Pregnancy Outcomes in Women after Surgery for Valvular Heart Disease
*Corresponding author: Nikhil Dixit, Department of Cardiothoracic Surgery, Nizams Institute of Medical Sciences, Punjagutta, Hyderabad, India. drdixitnikhil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Malempati AR, Palanki SS, Dixit N. A study of fertility and pregnancy outcomes in women after surgery for valvular heart disease. Indian J Cardiovasc Dis Women 2022;7:198-203.
Abstract
Objectives:
Chronic Rheumatic Heart Disease (CRHD)is a common condition in India. CRHD accounts for a majority of heart valve surgery, including those in the younger age group. These young women almost traditionally get married in a country like India, and the social pressure to bear children is tremendous. Anticoagulation and the postoperative state of the patient itself can be a risk factor for maternal and fetal outcomes. There is very little data available for the same in India.
Materials and Methods:
In this study, 100 cases were studied retrospectively to study the fertility patterns after valvular heart surgery including fetal outcomes. This study was conducted at Nizam’s Institute of Medical Sciences, Hyderabad in which pregnancy, anticoagulation, maternal and fetal outcomes were studied.
Results:
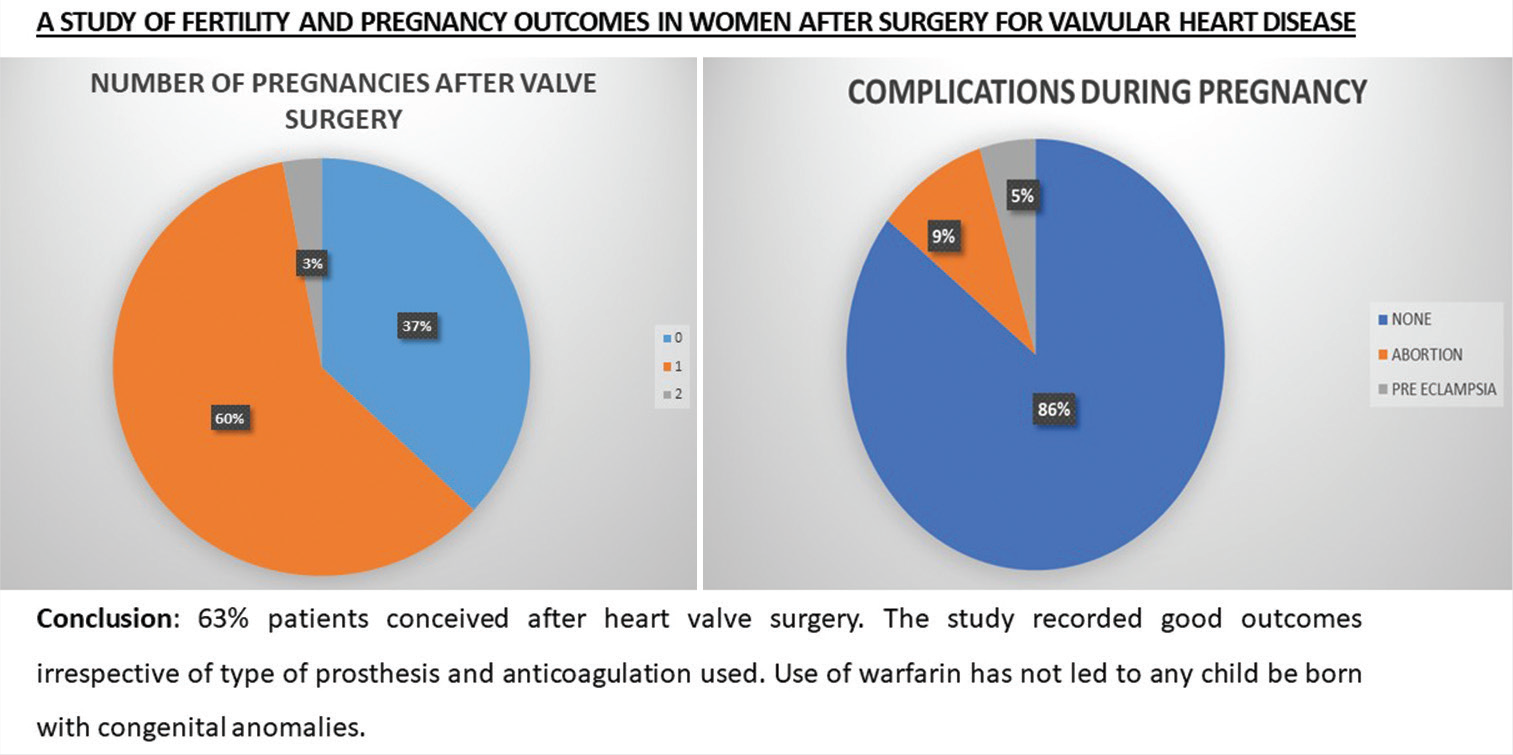
A total of 63 patients conceived after surgery (pregnancy rate = 63%/ failure rate =37%) (p=0.001). Fetal loss occurred in 6 of the pregnancies, due to spontaneous abortion (n=3) and medical abortion (n=3). Parity, associated conditions and age did not affect the outcome. During pregnancy, 28 patients switched to UF heparin, 31 stayed on warfarin, 4 did not take any anticoagulation. Fetal loss was observed in 3 patients on Warfarin during pregnancy and 3 on UF heparin. Maternal loss was observed in 4 patients out of which 2 were on Warfarin, 1 on unfractionated UF heparin and 1 did not take any anticoagulation during pregnancy. In comparison, warfarin and UF heparin had similar fetal outcomes.
Conclusion:
The study recorded good outcomes irrespective of type of prosthesis and anticoagulation.
Keywords
Anticoagulation
Fertility
Valve replacement
ABSTRACT IMAGE
INTRODUCTION
Chronic Rheumatic Heart Disease is common in India and a major cause for morbidity. It accounts for a majority of the heart valve surgeries in India.[1] Involvement in women is also quite high, and many young women undergo valvular heart surgeries, often replacement by mechanical heart valve prosthesis.[2] India is a country, where the women are expected to get married almost universally, and the pressure on these women to bear children is tremendous. Surgical options for valve replacement in young women, thus, throw up a unique set of dilemmas amidst our socioeconomic and cultural background.
The considerations guiding the choice of surgery include durability of valve repair v/s replacement surgery, need for one-time solution with mechanical prosthesis versus reoperations with a bioprosthesis later in life versus reoperation with a suboptimal repair to buy some time, and maternal and fetal risk for future child birth in view of medical condition of the patient as well as use of oral anticoagulation.
Decision-making regarding the choice of surgery offered to the patients is based on traditional beliefs and notions rather than hard data collected and validated in our Indian population, and keeping into perspective our social and cultural considerations. Anticoagulation and the post-operative state of the patient itself are reported to be risk factors for maternal and fetal outcomes.[3-5] Rheumatic population are usually not amenable for valve repairs. There is very little data which throws light on redo valve replacement surgeries following repairs specifically in the women within the reproductive age group. There are very little data to go by for valve replacement with a bioprosthetic valve in young age groups in this Indian population.
There is a serious gap in the knowledge of key parameters, and yet, decisions are made on the choice of surgery based on the assumption that.
All patients will get married and conceive
Warfarin embryopathy may occur in the fetus if a woman post mechanical valve replacement conceives without planning
All patients post mitral valve repair or replacement with a bioprosthesis will have normal outcomes of pregnancy.
We believe that crucial life defining decisions regarding choice of surgery and planning of a family in the future should not be based on assumptions, but rather on hard data in our socioeconomic and cultural context and this forms the basis of our study. The present study aims to study the fertility patterns in female patients in the reproductive age group who underwent valvular heart surgery, the maternal and fetal outcomes, and the clinical and therapeutic factors which influence the outcomes.
MATERIAL AND METHODS
The study is a retrospective study conducted at the Nizam’s Institute of Medical Sciences, Hyderabad. Women within the age group of 14 to 35 years who underwent valvular heart surgery between the years 2013 and 2019 were included in the study.
The Institute Ethics Committee approval was taken for the study. The information was obtained from case records and discharge records, and telephonic interviews.
The patients were studied for age, indications for surgery, type of surgery done, anticoagulation, incidence of pregnancy, and the maternal and fetal outcomes of the study.
The detailed reasons for infertility, maternal deaths, and loss of pregnancy were excluded from the study.
One hundred patients were taken as the sample size out of 187 patients [Figure 1]. These included all females in the reproductive age group (up to 35 years) who have undergone valvular heart surgery. Patients with concomitant surgeries and who were not married or desirous of childbirth after surgery were excluded from the study.
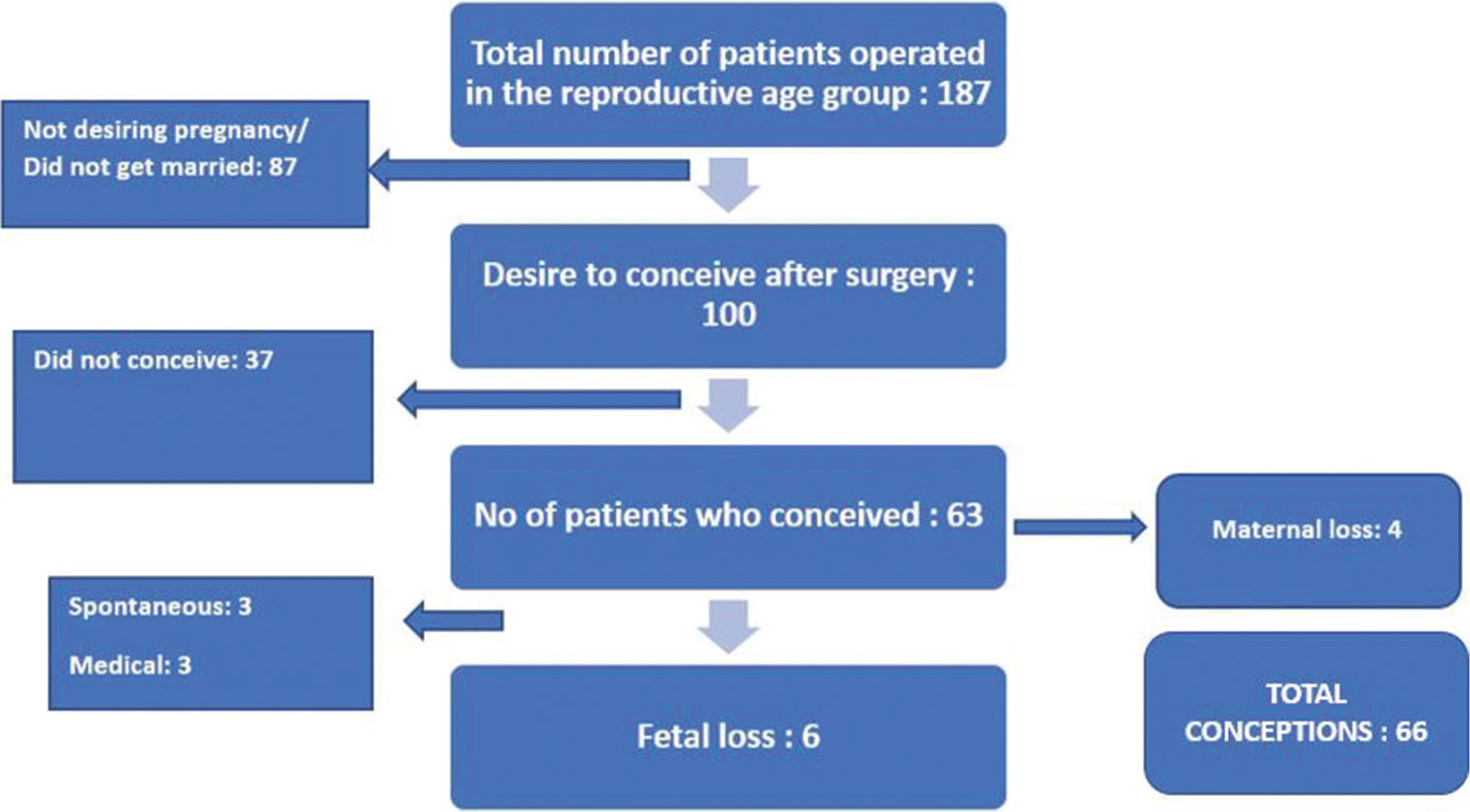
- Sample size flow chart.
Statistical analysis
Comparison done using Fishers exact test and Chi-square test after data was expressed as rates, ratios, and percentages. P value (probability) of less than or equal to 0.05 at 95% confidence interval was taken to be statistically significant.
RESULTS
The average age in the present study of 100 patients was 27.24 years. About 14% made up age range 16–20 years, 27% 21–25 years, 29% 26–30 years, and 30% 31–35 years. The average anticoagulation years were 3.98 years. The average years of marriage were 6.04 years out of which 57% comprised patients married for 1–5 years, 30% for 6–10 years, 11% for 11–15 years, and 2% for 16–20 years.
The total pregnancies ranged from zero (13%), one (42%), two (29%), and three (8%). The patients, who underwent mitral valve surgery was 63% and aortic valve surgery was 20%, had a combined double valve surgery 16% and 1% had only tricuspid valve surgery [Figure 2]. Thirty-seven patients out of 100 did not conceive. In the remaining 63 patients, 60 conceived once after surgery and three conceived twice after surgery [Figure 3].
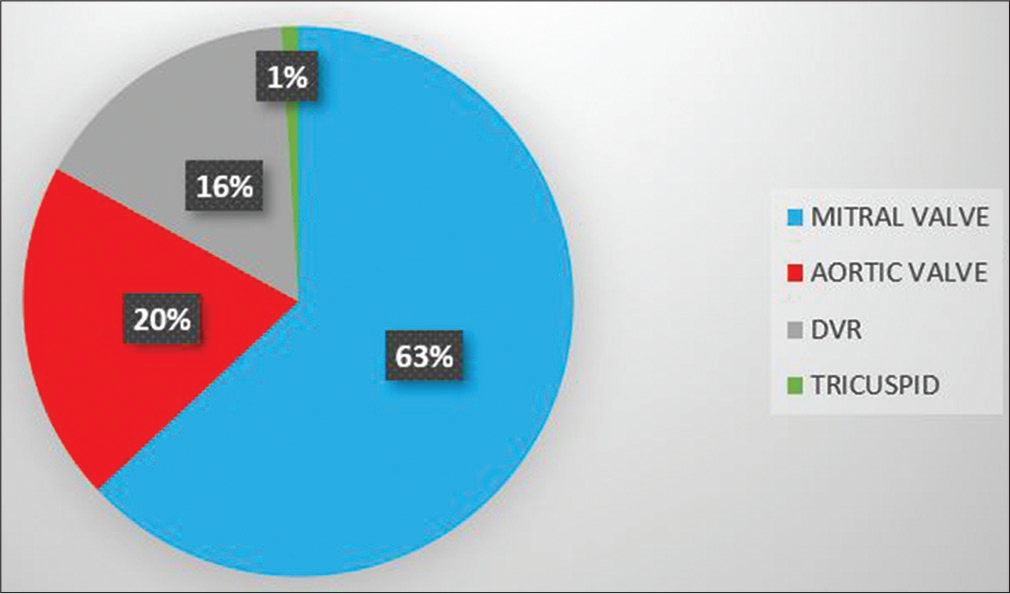
- Pie chart representing the various valve surgeries undertaken for the sample size.
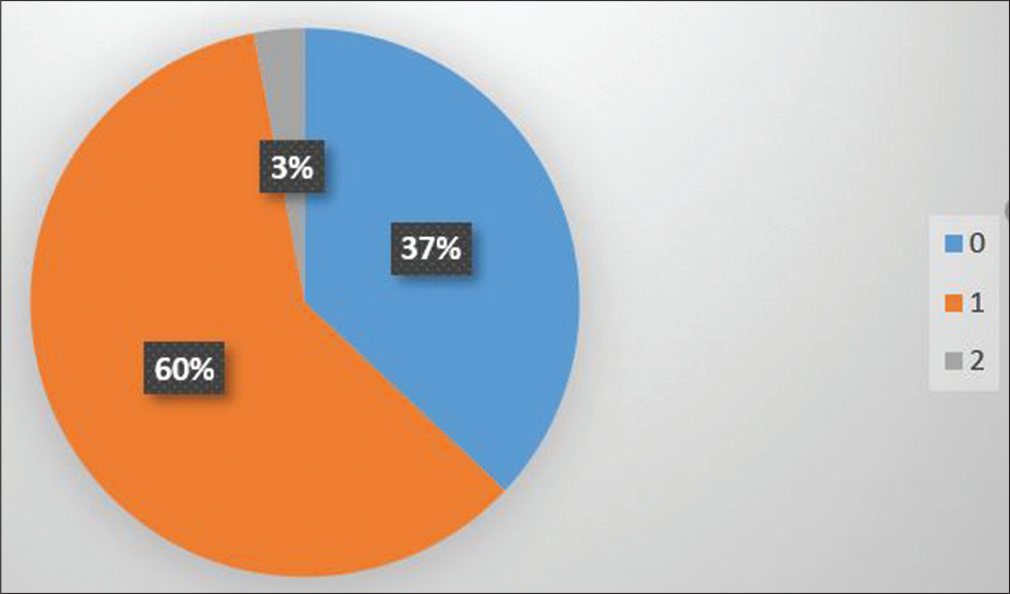
- Pie chart representing number of pregnancies attained after valve surgery.
The statistical analysis between pregnancies after surgery to pregnancy outcomes was as follows: P value was 0.001 which was statistically significant [Table 1]. About 9% had an abortion, out of which three were spontaneous and three were medical [Figure 4]. Four patients were on 5 mg warfarin, one on 3 mg, and the remaining one on 2 mg warfarin.
| Pregnancy outcomes | Total | Collective P value | |||
|---|---|---|---|---|---|
| Abortion | Birth | None | |||
| Pregnancy after surgery | 0.001 | ||||
| 0 | 0 | 0 | 37 | 37 | |
| 1 | 5 (8.30%) | 55 (91.70%) | 0 (0%) | 60 | |
| 2 | 1 (33.30%) | 2 (66.70%) | 0 (0%) | 3 | |
| Total | 6 (6%) | 57 (57%) | 37 (37%) | 100 | |
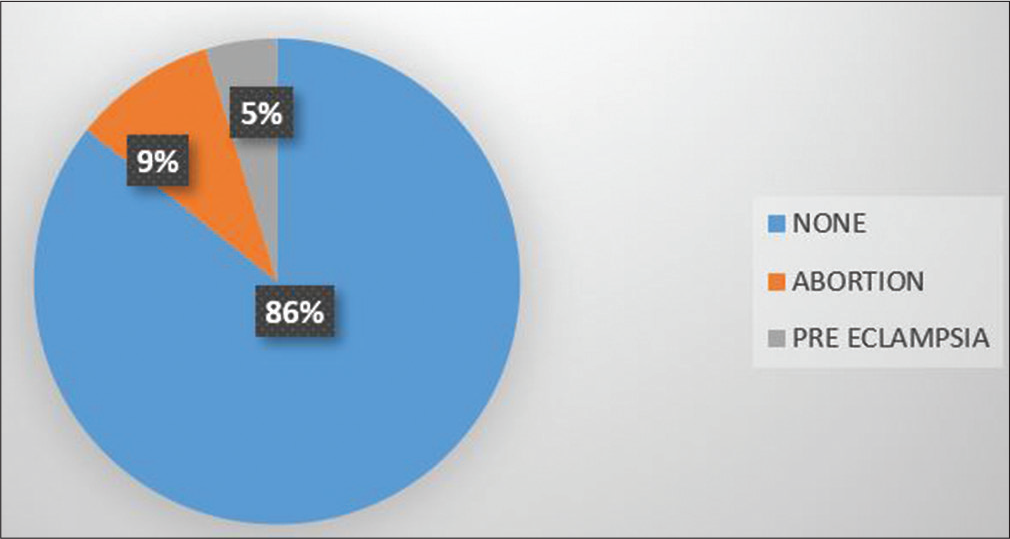
- Pie chart representing complications during pregnancy.
The statistical analysis between medication during pregnancy to condition of baby born was as follows: p value was 0.106 which was statistically insignificant [Table 2]. About 6.3% (n = 4) was the mortality recorded, out of which two were on Warfarin, one on UF heparin, and one did not take any anticoagulation during pregnancy. The patients had a brief hospitalization before decompensation. The details could not be studied.
| Condition of baby born | ||||
|---|---|---|---|---|
| Aborted | Healthy | Total | Collective P value | |
| Medication during pregnancy | 0.106 | |||
| Heparin | 2 (7.1%) | 26 (92.9%) | 28 | |
| None | 0 (0%) | 4 (100%) | 4 | |
| Unknown | 0 (0%) | 4 (100%) | 4 | |
| Warf | 4 (14.8%) | 23 (85.2%) | 27 | |
| Total | 6 (9.5%) | 57 (90.5%) | 63 | |
The statistical analysis between pregnancies after surgery to maternal mortality was as follows: P value was 0.047 which was statistically insignificant [Table 3]. Two had undergone a mitral valve replacement, one had undergone mitral valve replacement with tricuspid repair, and one had undergone redo mitral valve replacement. Two patients were on 5 mg warfarin, one on 7.5 mg warfarin, and the remaining one was on 2 mg warfarin.
| Mortality | Total | Collective P value | ||
|---|---|---|---|---|
| No | Yes | |||
| Pregnancy after surgery | 0.047 | |||
| 1 | 57 (95%) | 3 (5%) | 60 | |
| 2 | 2 (66.7%) | 1 (33.3%) | 3 | |
| Total | 59 (93.6%) | 4 (6.4%) | 63 | |
There were no obvious genetic anomalies detected with the other deliveries at term and the children were healthy.
DISCUSSION
In a developing country like India, chronic rheumatic heart disease is rampant and it affects mainly the young population. Out of them, many are young women who need valvular heart surgeries and often undergo replacement of a heart valve. These young women almost universally get married in a country like India, and the social pressure to bear children is tremendous.
Usually, high-risk patients are young women planning pregnancy. The selection of the type of prosthesis should be done by adhering to the current AHA and ESC guidelines. The preferable valve choice, according to these guidelines, for this group is bioprosthesis.[6] However, future dysfunction of the bioprosthesis requires reinterventions in this group.
Mechanical valves, on an average, have a lifespan of around 20–30 years, which makes it ideal for a younger demographic. Whereas, on the other hand, bioprosthetic heart valves have an average lifespan of around 8–15 years and depend on various factors such as prosthesis type, age, and position.[6] It was in 1966 that the first case of successful management of a patient with a prosthetic mitral valve which led to a successful delivery was reported. The concept of embryopathy due to warfarin was first defined by Hall in 1965.[7]
It has been found that congenital malformations in the fetus are caused by crossing of the placental barrier by orally administered agents, which achieve satisfactory anticoagulation. UF heparin and its other fractionated formulations do not cross the placental barrier; despite this, they are not as potent as oral anticoagulants in preventing complications like stroke in the mother.
A study with a 30-year follow-up was conducted in Denmark. This study group included pregnant women who had undergone prosthetic heart valve surgery. The study postulated that fetal and maternal complications were associated with anticoagulant therapy.[8] The accurate prevalence and incidence of warfarin embryopathy are tough to establish. The reported numbers range from less than 5 % to more than 67 % in various studies; whereas a range of 4 to 10 % has been described by other researchers.[9]
Managing pregnancy in patients with mechanical valves is a debatable issue. The current ACC/AHA guidelines advocate three strategies.[10] First is Warfarin continued throughout pregnancy at doses <5 mg/day.[11] A recent meta-analysis showed that at these dosages, the fetal toxicity risk is much lower.[12] The second strategy is usage of heparin and analogues throughout pregnancy.[10] When the target INR exceeds 5 mg, LMWH or UFH is recommended. However, LMWH is completely metabolized by the kidneys and, hence, underperforms.[13] The third potential strategy is the usage of sequential therapy, where heparin is used in the first trimester and warfarin in the remaining two.[10] The rate of loss of fetus in women with prosthetic heart valves ranges from 8.5% to 66% in various evaluations.[14,15] In a study comparing pregnancy outcomes in women with mechanical prosthesis on warfarin therapy to patients on UF heparin therapy, it was found that the rate of fetal loss was 53% on warfarin therapy, 36% on UF heparin, and 16.7% without use of any anticoagulant. However, in a report published in Nigeria, out of the total two cases, one patient had two successful pregnancies, in spite of not being compliant on warfarin and the other had a successful delivery while on heparin therapy.[16] This study concludes that in a low socioeconomic setting, the main issues are inadequate anticoagulation and monitoring.
In our study, the fetal loss was 9%, of which only 50% was spontaneous. All of the fetal loss was seen in the first trimester. However, all pregnancies which were carried till term were normal. Therefore, we may consider that while a clear risk of losing a defective fetus exists, it is less than that reported in the literature. Furthermore, the conventionally reported risk of a child being born with congenital malformations requires reassessment. In our study, all the patients who underwent spontaneous abortions had a warfarin dose of 5 mg. No meaningful interpretation can be made out regarding the correlation of the dose of warfarin and spontaneous abortion.
Neither the age of the mother at the time of pregnancy nor the interval between the operation and pregnancy had any effect on the outcome.
Controversy exists in the usage of warfarin therapy in the pregnancy’s first trimester. It is considered teratogenic. Reports recently published have showed that warfarin embryopathy is a tremendously infrequent occurrence[17,18] and that loss of the fetus may be dependent on the dosage of warfarin.[19] There also have been studies that even UF heparinization delivers insufficient anticoagulation, which puts a risk for valvular malfunction and thromboembolism to the mother.[20,21] In our study, six patients who had fetal loss among them three were on warfarin during their pregnancies and three were on UF heparin. Theoretically, thromboembolism can occur in patients who are on UF heparin during pregnancy especially the first trimester. Hence proving that UF heparin provides inadequate protection in these patients against thromboembolism, similar to conclusions by other researchers. In the present study, excluding one patient who had bleeding during delivery (? postpartum hemorrhage) others had no complications. The patients, thus, irrespective of the choice of surgery and prosthesis, duration, and dose of anticoagulation, had good outcomes.
CONCLUSION
About 63% patients conceived after heart valve surgery. Significant majority of cases failed to either get married or decide against pregnancy at the initial time of surgery, thereby making a therapeutic choice irrelevant.
The study recorded good outcomes irrespective of type of prosthesis and anticoagulation used. The use of warfarin has not led to any child be born with congenital anomalies.
Limitations
This is a retrospective study. The bioprosthetic group in this study is small. The study has not evaluated medical cause of infertility (maternal or paternal). The study has not evaluated the aborted fetuses for genetic anomalies.
Recommendations
Guidelines in Indian context need to be rewritten. Larger multicentric prospective studies need to be done to generate clear data for proper counseling. The fallacy that oral anticoagulation leads to babies being born with congenital anomalies should be corrected. A clear plan of pregnancy should be taken into account when considering options like suboptimal repair or bioprosthetic valve replacement which entails high-risk redo surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Audio summary available at
https://doi.org/10.25259/mm_ijcdw_459
References
- Valvular heart disease in Indian subcontinent: Social issues. Indian J Community Med. 2009;34:57-8.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and patterns of valvular heart disease in a tertiary care high-volume cardiac center: A single center experience. Indian Heart J. 2014;66:320-6.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of pregnancy in women with mechanical valves. Tex Heart Inst J. 2000;27:240-5.
- [Google Scholar]
- Anticoagulant choices in pregnant women with mechanical heart valves: Balancing maternal and fetal risks--the difference the dose makes. Thromb Res. 2013;131:S8-10.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of valve surgery on female fertility. Gynecol Obstet Invest. 1992;34:184-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac crossroads: Deciding between mechanical or bioprosthetic heart valve replacement. Patient Prefer Adherence. 2011;5:91-9.
- [CrossRef] [PubMed] [Google Scholar]
- Embryopathy associated with oral anticoagulant therapy. Birth Defects Orig Artic Ser. 1976;12:33-7.
- [Google Scholar]
- Pregnancy with prosthetic heart valves-30 years' nationwide experience in Denmark. Eur J Cardiothorac Surg. 2011;40:448-54.
- [CrossRef] [PubMed] [Google Scholar]
- Prosthetic heart valves and pregnancy. Circulation. 2003;107:1240-6.
- [CrossRef] [PubMed] [Google Scholar]
- 2020 ACC/AHA Guideline for the management of patients with valvular heart disease: A report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 2021;143:e72-227.
- [CrossRef] [Google Scholar]
- Anticoagulation during pregnancy: Evolving strategies with a focus on mechanical valves. J Am Coll Cardiol. 2016;68:1804-13.
- [CrossRef] [PubMed] [Google Scholar]
- Anticoagulation regimens during pregnancy in patients with mechanical heart valves: A systematic review and meta-analysis. Can J Cardiol. 2016;32:1248.e1-1248.e9.
- [CrossRef] [PubMed] [Google Scholar]
- Low molecular weight heparin for the prophylaxis of thromboembolism in women with prosthetic mechanical heart valves during pregnancy. Thromb Haemost. 2004;92:747-51.
- [CrossRef] [PubMed] [Google Scholar]
- Is there a safe anticoagulation protocol for pregnant women with prosthetic valves? Clin Exp Obstet Gynecol. 1998;25:101-4.
- [Google Scholar]
- Guidelines for prevention of thromboembolic events in valvular heart disease. Study group of the working group on valvular heart disease of the European Society of cardiology. Eur Heart J. 1995;16:1320-30.
- [CrossRef] [PubMed] [Google Scholar]
- Anticoagulation in pregnant women with mechanical heart valve prostheses: Case reports and a literature review. Niger Postgrad Med J. 2021;28:68-70.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of pregnancy in women with valve prostheses. Br Heart J. 1994;71:196-201.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnancy in patients with prosthetic cardiac valve. A 10-year experience. Scand J Thorac Cardiovasc Surg. 1988;22:19-22.
- [CrossRef] [PubMed] [Google Scholar]
- Dose-dependent fetal complications of warfarin in pregnant women with mechanical heart valves. J Am Coll Cardiol. 1999;33:1637-41.
- [CrossRef] [PubMed] [Google Scholar]
- Failure of adjusted doses of subcutaneous UF heparin to prevent thromboembolic phenomena in pregnant patients with mechanical cardiac valve prostheses. J Am Coll Cardiol. 1996;27:1698-703.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnancy after cardiac valve replacement: Analysis of 21 cases [in Chinese] Chung Hua Fu Chan Ko Tsa Chih. 1993;28:386-8, 440
- [Google Scholar]








