Translate this page into:
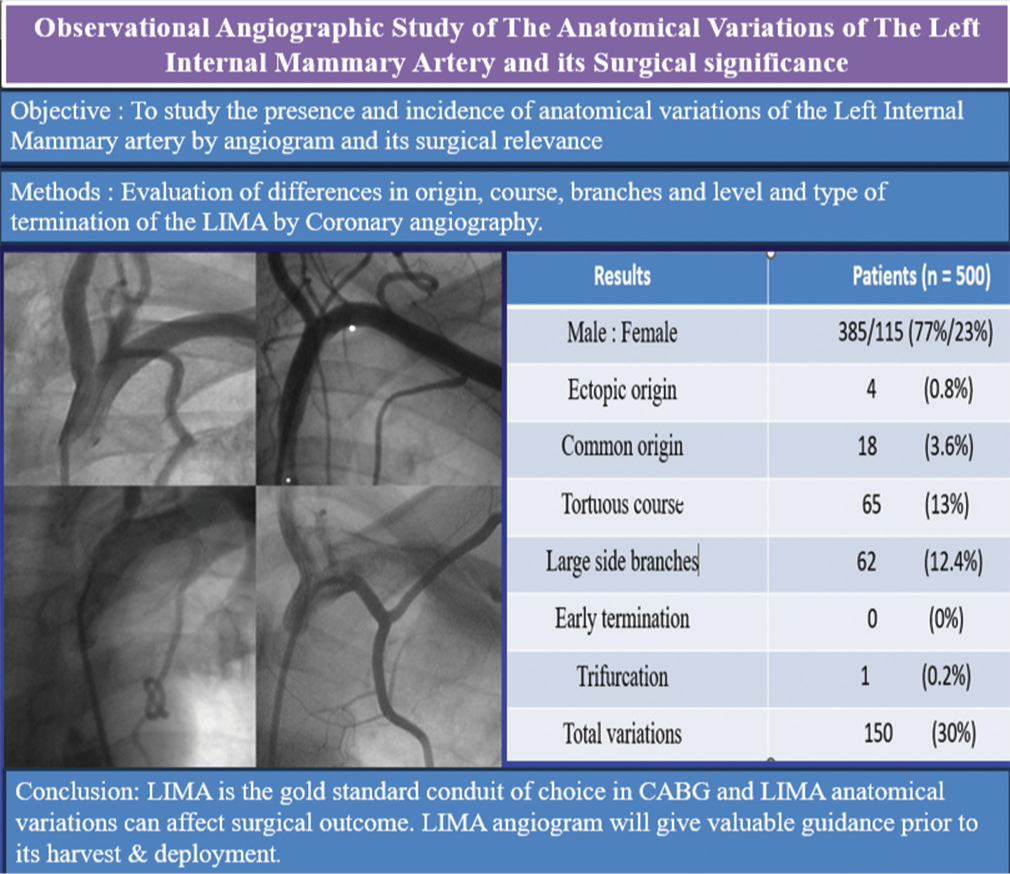
Observational Angiographic Study of the Anatomical Variations of the Left Internal Mammary Artery and its Surgical Significance
*Corresponding author: R. Subathra Devi, Department of Cardiothoracic Vascular Surgery, Apollo Hospitals, Chennai, Tamil Nadu, India. subathra.genga@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Devi RS, Nayak R, Viswanath A, Mishra DK. Observational Angiographic Study of the Anatomical Variations of the Left Internal Mammary Artery and its Surgical Significance. Indian J Cardiovasc Dis Women. 2025;10:36-40. doi: 10.25259/IJCDW_33_20 24
Abstract
Objective:
The objective of this study was to study the presence and incidence of anatomical variations of the left internal mammary artery (LIMA) by angiogram and its surgical relevance.
Materials and Methods:
In patients with coronary artery disease, who were referred for coronary artery bypass grafting (CABG), we evaluated the LIMA while performing coronary angiogram. The study involved evaluation of differences in origin, course, branches, and level and type of termination of the LIMA.
Results:
LIMA was assessed angiographically in 500 patients who underwent CABG surgery. Anatomical variations were observed in 150 patients (30%). Ectopic origin of LIMA from the third part of the Subclavian artery was seen in 3 patients (0.6%). Eighteen patients (3.6%) had common origin of LIMA from thyrocervical trunk. LIMA had a tortuous course with loops and bends in 65 cases (13%). A large lateral costal branch from the proximal part of LIMA supplying the lateral chest wall was seen in 60 cases (12%). In all patients, LIMA was found to terminate as a bifurcation at or beyond the 6th rib.
Conclusion:
Angiographic evaluation of the LIMA can highlight the anatomical variations of the LIMA thereby forewarns and enables the surgeon to make a safe harvest of the LIMA. LIMA is the primary conduit of choice for CABG operations due to the longevity of the conduit. If a prominent lateral costal branch is left unclipped, it may cause internal mammary artery steal. Ectopic origin and tortuous course can endanger the LIMA during harvest. Prior knowledge of the LIMA variations visualized during angiogram will enable the surgeon to anticipate and take adequate precautions for a safe LIMA harvest.
Keywords
Left internal mammary artery
Anatomical variations
Coronary angiography
Coronary artery bypass grafting
Left internal mammary artery course
ABSTRACT IMAGE
INTRODUCTION
Coronary bypass grafting is the surgical revascularization of the ischemic myocardium with native conduits such as internal mammary artery (IMA), radial artery, and saphenous vein grafts (SVG). The IMA is resistant to atherosclerosis and has excellent long-term patency rate of 95% at 10 years when compared to rheumatoid arthritis (83%) and SVG (81%).[1]
The left IMA (LIMA) takes its origin, as an isolated artery, from the first part of the subclavian artery opposite the thyrocervical trunk.[1] Occasionally, it takes an ectopic origin from the second or third part of the subclavian artery. It can arise as a common trunk with either the inferior thyroid, transverse cervical or dorsal scapular arteries.
The course of the LIMA is usually straight and parallel to the sternal margin, but it can be tortuous, acutely angled, or looped. The site of termination is usually at the sixth intercostal space but can rarely be either in the space above or below. It bifurcates into two terminal branches, the superior epigastric artery and musculophrenic artery but rarely trifurcation occurs. A side branch is considered large when it is more than half the width of the main artery.
Standard anatomy and variations of the IMA have been studied by cadaver dissections. Knowledge of these variations, although few, become surgically significant at the time of IMA harvest and prevention of recurrence of angina.
MATERIALS AND METHODS
We studied the LIMA by angiography in 500 patients with coronary artery disease who had coronary angiograms before their coronary artery bypass grafting (CABG). Anatomical variations of the site and type of origin, nature of course, site and type of termination, and large side branches were evaluated in all cases.
RESULTS
Among the 500 cases evaluated in this study, 77% were male (385/500) and 23% were female (115/500). About 63% (315/500) cases were hypertensive. About 34% (170/500) were chronic smokers.
The left internal mammary was present and visualized angiographically in all patients involved in the study. We had encountered a total of 30% (150/500) anatomical variations of LIMA in our study, as described in Table 1. About 58% (87/150) patients with LIMA abnormalities were male and 42% (63/150) were female. Among the 115 female patients in the study, 54.78% (63/115) had LIMA anatomical variations. About 22.6% (87/385) male had LIMA variations.
| Anatomical variations | Number n(%) |
|---|---|
| Ectopic origin | 4 (0.8) |
| Common origin | 18 (3.6) |
| Tortuous course | 65 (13) |
| Large side branches | 62 (12.4) |
| Early termination | 0 (0) |
| Trifurcation | 1 (0.2) |
| Total | 150 (30) |
LIMA: Left internal mammary artery
Out of the 150 patients with LIMA abnormalities, 85.33% (128/150) were hypertensive and remaining (22/150–14.67%) were normotensive. Hence, hypertensive patients had more incidences of LIMA abnormalities than normotensive patients.
The LIMA originated as an independent artery from the subclavian artery in 96.4% (482/500) cases and as a common truck with suprascapular, inferior thyroid, and transverse cervical arteries in 3.6% (18/500) cases, as shown in Table 2 and Figure 1.
| Site and type of origin | Patients (n=500%) |
|---|---|
| 1st part of subclavian artery | 496 (99.2) |
| 2nd part of subclavian artery | 1 (0.2) |
| 3rd part of subclavian artery | 3 (0.6) |
| Independent origin | 482 (96.4) |
| Common origin | 18 (3.6) |
LIMA: Left internal mammary artery
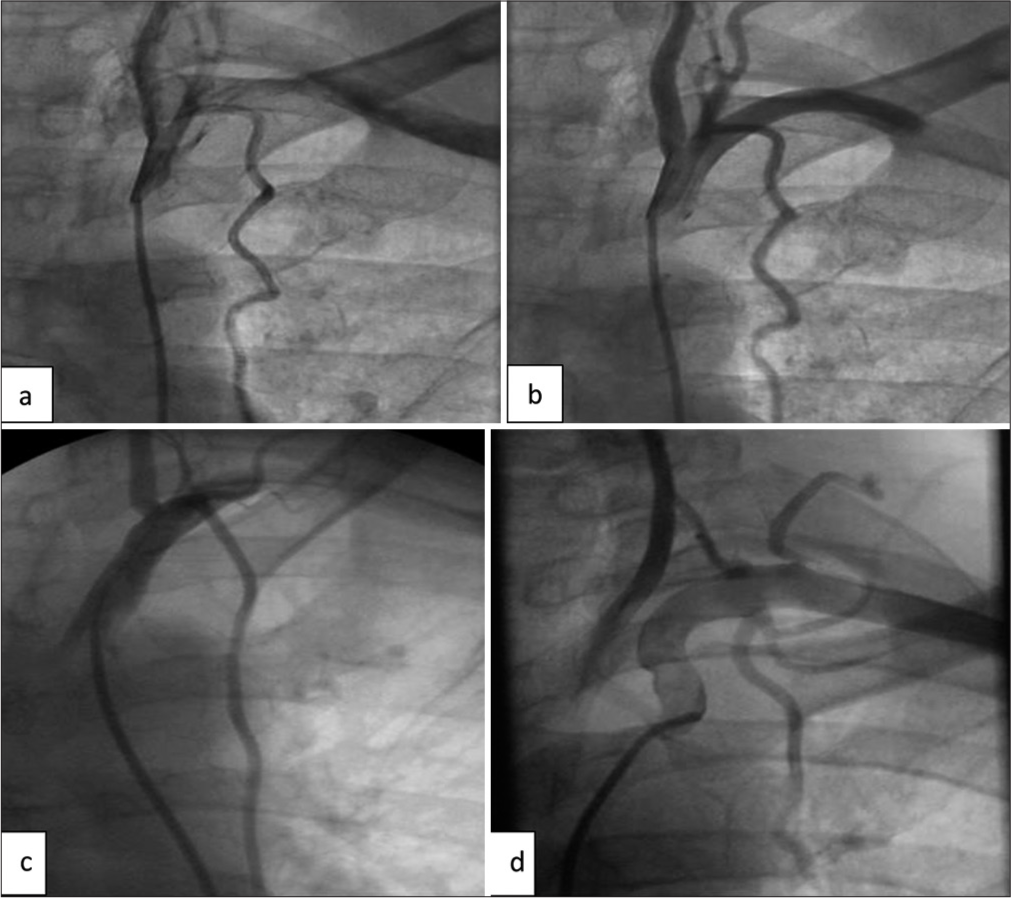
- Common origin of the LIMA. (a and b) LIMA arising as a common origin with Thyrocervical trunk. (c) common origin of LIMA with costocervical trunk. (d) Common origin of LIMA with dorsal scapular artery. (LIMA: Left internal mammary artery.)
In 99.2% (496/500) cases, the LIMA originated from the 1st part of the subclavian artery, 0.2% (1/500) case from the 2nd part, and 0.6% (3/500) cases from the 3rd part of the subclavian artery, as shown in Figure 2.
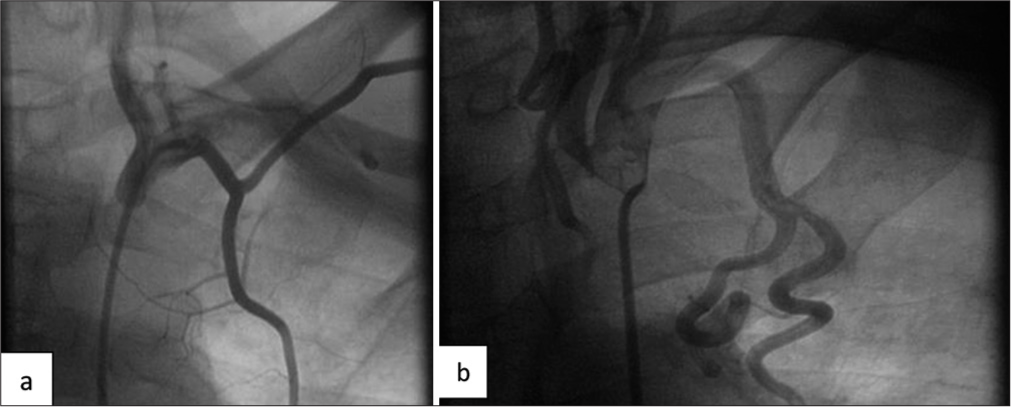
- Ectopic origin of the LIMA. (a and b) Ectopic origin of the LIMA arising from the 3rd part of subclavian artery. (b) Acute angulation of LIMA. (LIMA: Left internal mammary artery.)
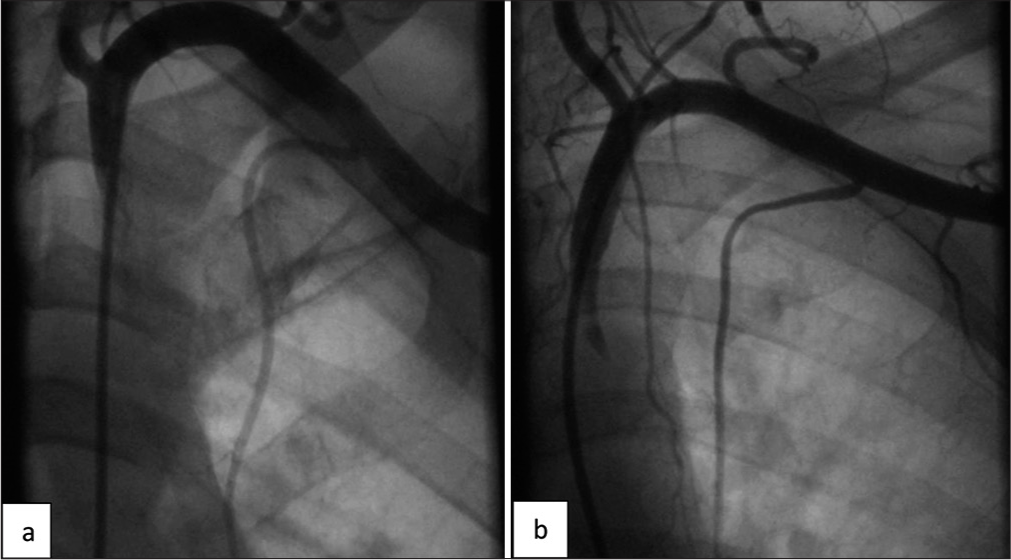
The LIMA had a predominantly linear vertical course (87%– 435/500). The remaining 13% (65/500) had a tortuous course, as shown in Figure 3. The tortuosity was further subcategorized as kinks, loops, and coils. Among the 65 cases, 61.5% (40/65) had kinks, 27.7% (18/65) had loops, and 10.8% (7/65) had coils. None of the LIMA had an atypical course, as shown in Table 3.
- Tortuous course of LIMA. (a-d) Tortuous course of LIMA with kink, loop, and coils. (a) Kinking. (b) Looping of LIMA. (c and d) Coiling of the LIMA. (LIMA: Left internal mammary artery.)
| Nature of course | Patients (n=500%) |
|---|---|
| Linear | 435 (87) |
| Tortuous course | 65 (13) |
| Kinks | 40 (61.5) |
| Loops | 18 (27.7) |
| Coils | 7 (10.8) |
LIMA: Left internal mammary artery
The level of termination of the LIMA was at the 6th intercostal space in majority of the cases (85%–425/500) and at the 6th rib in the remaining 15% (75/500) cases. In our study, we have not encountered any early termination of LIMA.
The type of termination has been a bifurcation in 99.8% (499/500) cases, with an exception of one case where it was a trifurcation.
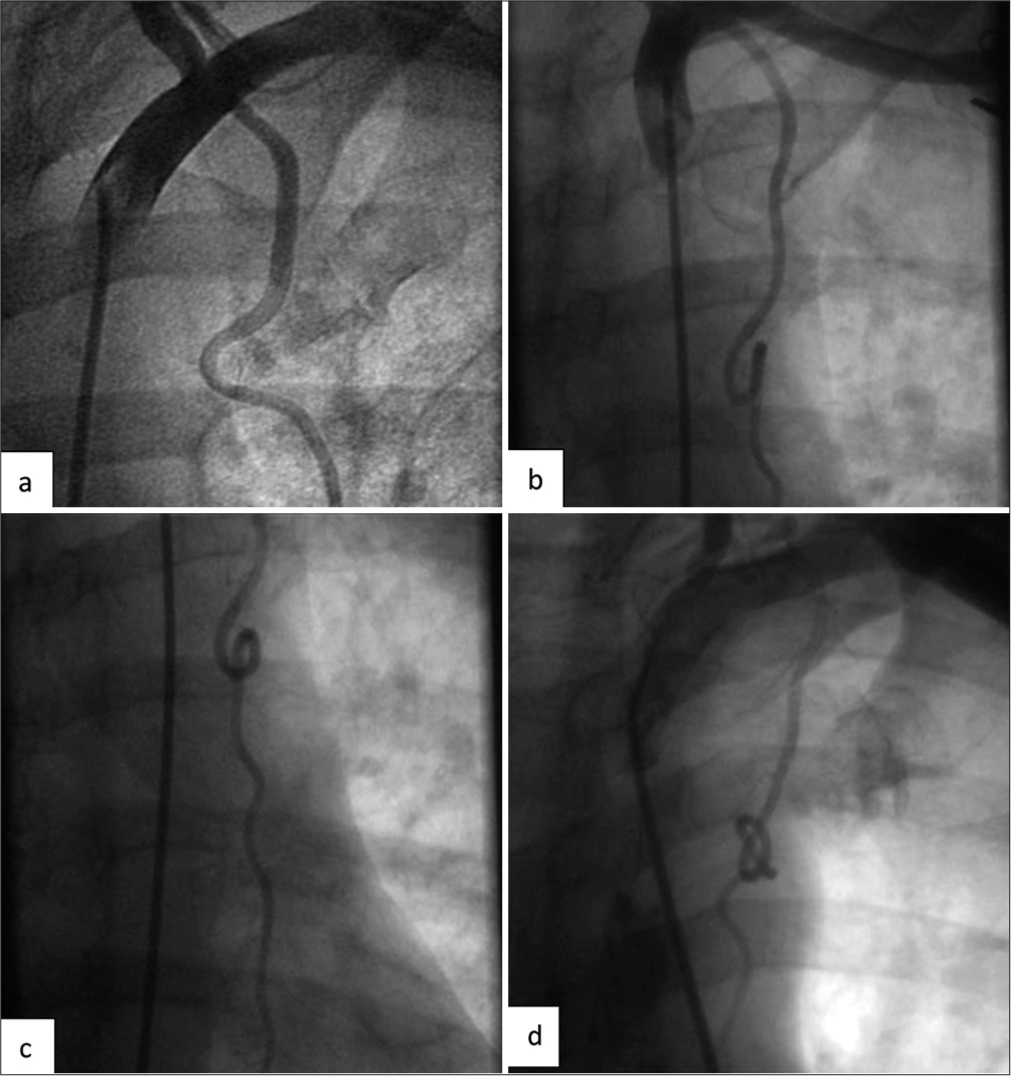
The lateral costal branch was seen in 12% (60/500) cases and a large medial branch was present in 0.4% (2/500) cases, as shown in Figure 4.
- Large side branch of LIMA. (a and b) Large costal branches arising from the lateral aspect of LIMA. (LIMA: Left internal mammary artery.)
All the 500 LIMA conduits were used as bypass graft after meticulous harvesting.
DISCUSSION
A total of 30% (150/500) patients involved in the study were found to have anatomical variations of the LIMA. Among these 150 patients, 42% were female (63/150), out of whom 92.06% (58/63) females were hypertensive. A total of 128 patients who had LIMA variations were hypertensive. Most commonly encountered variations of LIMA include tortuous course 43.33% (65/150), large lateral costal branch 41.33% (62/150), and common origin 12% (18/150). About 99.2% (496/500) of the LIMA arose from the 1st part of subclavian artery. Only one had trifurcation of LIMA at termination (0.66%) and there was no incidence of early termination.
Among all the conduits for CABG, the LIMA is the gold standard conduit.[1]
Anatomical variations of the LIMA exist, with an incidence of 30% (present study and Bauer et al.).[2] Prior knowledge of these variations is surgically significant for safe harvest and usage of the LIMA as a bypass graft.
LIMA arises usually from the 1st part of the subclavian artery. Rarely, it may also arise from the 3rd part of the subclavian artery with a reported incidence of 1% as shown in the cadaveric study by Henriquez-Pino et al.,[3] 1.5% in the angiographic study by Bauer et al.,[2] and 0.6% in our present study. LIMA with lateral origin can potentially get injured at the level of the 1st rib during harvest and due to the angulation, can get stretched with compromised flow following grafting.[4]
LIMA usually arises as an independent artery but occasionally arises as a common trunk with other arteries with incidence of 30% by Henriquez-Pino et al., 12.2% by Bauer et al., and 3.6% in our present study.[2,3] In these cases, there is a possibility of steal phenomenon with recurrence of angina in the post-operative period as demonstrated by Tartini et al. and Paraskevas et al.[5,6]
Arterial tortuosity is related to vascular elongation due to aging, hypertension, and genetics. Weibel and Fields classified the arterial tortuosity into kinking, looping, and coiling.[7] Kinking is described as an acute angulation, looping as a smooth S or C shaped curve and coiling as a circular 360° in the vessel. Incidence of tortuosity as per Henriquez-Pino et al. was 7%, Bauer et al. was 6.1%, and Agnihotri and Mitra was 10%.[2,3,8] In our present study, 13% had tortuous course. These tortuous LIMA are more susceptible to injury at the time of harvest.
In our study, none of the LIMA had early termination, with all of them terminating either at or beyond the 6th rib and hence the length of the LIMA was sufficient for grafting.
Lateral costal branch arising at the level of the 1st rib was present in 15% cases of Henrique-Pino et al.,[3] 8.8% cases of Bauer et al.,[2] and 12% cases of our study. Un-ligated lateral costal branch has been documented to cause recurrent angina due to IMA steal phenomenon necessitating either transcatheter coil obliteration or video-assisted thoracoscopic surgery ligation by Pagni et al.[9]
With the presence of LIMA anatomical variations, we had to modify our surgical strategy. In cases of LIMA with common origin, we may have to divide the thyrocervical trunk through a supraclavicular approach or we may have to use a saphenous vein conduit instead of the IMA. Meticulous harvest is mandatory when there is a lateral origin and tortuous course of LIMA. Lateral costal branch should be identified, then ligated, and divided in continuity.
CONCLUSION
Our study shows that during coronary angiography, if significant coronary artery disease is identified, angiography of the LIMA should be performed. This imaging will help in identification of surgically significant anatomical variations of the LIMA. Surgical strategy can be modified for a safer LIMA harvest with prior knowledge of the anatomy.
Ethical approval
The Institutional Review Board approval is not required as it is an observational study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship: Nil.
References
- Influence of the Internal-Mammary-Artery Graft on 10-Year Survival and other Cardiac Events. N Engl J Med. 1986;314:1-6.
- [CrossRef] [Google Scholar]
- Internal Mammary Artery Anomalies. Thorac Cardiovasc Surg. 1990;38:312-5.
- [CrossRef] [Google Scholar]
- Surgical Anatomy of the Internal Thoracic Artery. Ann Thorac Surg. 1997;64:1041-5.
- [CrossRef] [Google Scholar]
- Aberrant Left Internal Thoracic Artery Origin from the Extrascalenic Part of the Subclavian Artery. Exp Clin Cardiol. 2011;16:62-4.
- [Google Scholar]
- Anomalous origin of the left thyrocervical trunk as a cause of residual pain after myocardial revascularization with internal mammary artery. Ann Thorac Surg. 1985;40:302-4.
- [CrossRef] [Google Scholar]
- Abnormal Origin of Internal Thoracic Artery from the Thyrocervical Trunk: Surgical Considerations. J Cardiothorac Surg. 2012;7:63.
- [CrossRef] [Google Scholar]
- A Study on Origin, Termination, and Course Characteristics of Internal Thoracic Artery Relevant to Coronary Surgeries and Reconstructive Procedures. Tzu Chi Med J. 2021;34:348-52.
- [CrossRef] [Google Scholar]
- Successful VATS Ligation of a Large Anomalous Branch Producing IMA Steal Syndrome After MIDCAB. Ann Thorac Surg. 2001;71:1681-2.
- [CrossRef] [Google Scholar]








