Translate this page into:
Unraveling the Spectrum of Hypertension among Adult Women in an Urban Area of North India through Level of Prevention-based Color-coded Stratification
*Corresponding author: Amarjeet Singh, Head, Community Medicine and School of Public Health, Post Graduate Institute of Medical Education and Research, Chandigarh, India. dramarjeet56@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar P, Kumar R, Agrawal N, Khan AA, Arun R, Singh A. Unraveling the Spectrum of Hypertension among Adult Women in an Urban Area of North India through Level of Prevention-based Color-coded Stratification. Indian J Cardiovasc Dis Women. 2024;9:22-7. doi: 10.25259/IJCDW_57_2023
Abstract
Objectives:
The objective of this study was to investigate the prevalence of hypertension (HTN) in adult females at the Urban Health Training Center (UHTC) of a private medical college using a color-coded stratification based on levels of prevention.
Materials and Methods:
This cross-sectional study was conducted during June–July 2023 at UHTC, a private medical college. The sample size was calculated as 256. First, a basic health assessment of the study population was done. This focused on basic socio-demographic data of the adult women, their health status and blood pressure reading, risk profile, treatment-seeking behavior, etc. A proforma was developed to record the data. The principal investigator did a level of prevention-based color-coded stratification for HTN patient segmentation.
Results:
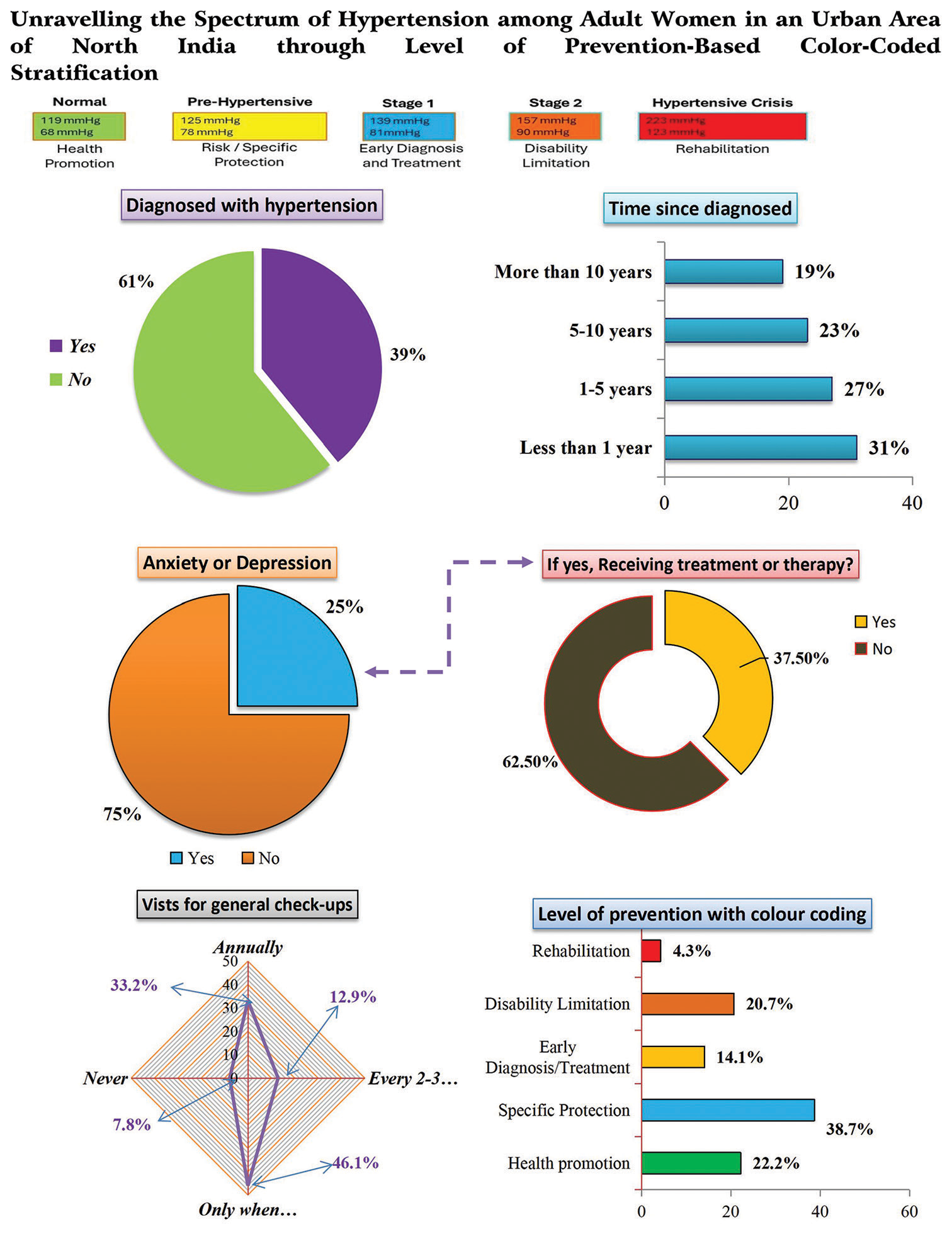
The majority of respondents were married (75.4%). Their literacy rate was 72%. The majority of the respondents were homemakers (58.2%). The mean age of the respondents was 38.23 years (range 18–75 years). Monthly household income ranged from Rs. 1,000 to 60,000, with a mean of Rs. 10,611.72. The average family size was 4.61 members. Some (22%) of the respondents fell into the “Health promotion” category (Green), indicating that they were free of HTN. About 39% of respondents were categorized under “Specific protection” (Blue), signifying that they were at risk of developing HTN; 14% were diagnosed with HTN cases without apparent complications, classified as “Early Diagnosis/Treatment” (Yellow). About 21% of respondents were placed in the “Disability Limitation” (Orange) category, indicating some complications, while 4.3% were identified as HTN patients needing “Rehabilitation” (Red) due to serious complications.
Conclusion:
This approach of the color-coded stratification based on levels of prevention among adult females of UHTC revealed the spectrum of HTN in the general community. Overall, 39% of the respondents had HTN. About two-fifths of respondents were at risk of developing HTN. This method has the potential to enhance the individualized management of HTN.
Keywords
Hypertension
Level of prevention
Color-coded stratification
Patient segmentation
Cardiovascular diseases
ABSTRACT IMAGE
INTRODUCTION
The prevalence of cardiovascular diseases (CVDs) such as hypertension (HTN), atherosclerosis, stroke, and myocardial infarction increases with age in both men and women.[1] It exerts a substantial public health burden on healthcare systems, as it is responsible for 57% of all stroke deaths and 24% of all coronary heart disease deaths in India.[2]
According to the WHO, one of the major global causes of premature death is high blood pressure.[3] Only 10–25 % of Indian HTN population have their blood pressure (BP) under control.[4] The low awareness and treatment levels among hypertensive patients signify poor knowledge, attitude, and practice levels among patients. The current mass-level strategies to control BP among Indian HTN patients are not working. These findings have enormous public health significance for policymakers and physicians alike.
There is a need to foster a conducive communication ambiance to convince HTN patients to take the treatment prescribed by the concerned physician.
At the grassroots level, there is a need to adopt a simple approach, which a primary health care worker can use comfortably. A color-coded client segmentation approach can be useful for HTN control in a community setting. Easy interface and color codes are recognized not only by the health care professionals but also by the caretakers irrespective of their educational status.
Risk profiling of HTN patients can be facilitated by color-coded health cards using standard risk prediction charts. Their language needs to be easy for better understanding by the patients. Such an approach will help in planning appropriate management.[5-10] This will help in averting cardiovascular deaths.
This will also be in tandem with the current focus of healthcare providers on an individualized patient-centered approach.
The color-coded approach has been in use in our health system for long. This system has been useful in many ways.
The use of such a color coding system in chronic diseases has tremendous potential for ensuring good quality health service delivery, especially in poor resource settings where chronic disease burden is high.
Objective
The objective of this study was to investigate the prevalence of HTN in adult females at the Urban Health Training Center (UHTC) of a private medical college using a color-coded stratification based on levels of prevention.
MATERIALS AND METHODS
This was a cross-sectional study conducted during June–July 2023 at UHTC of a private medical college. The sample size was calculated as 256 (n = 4PQ/d2).
A level of prevention-based color-coded stratification was done by the principal investigator (PI) for patient segmentation.
Inclusion criteria
The following criteria were included in the study:
Adult women visiting the outpatient department (OPD) of UHTC.
Exclusion criteria
The following criteria were excluded from the study:
Adult women not willing to participate
Pregnant women and extremely ill people (bedridden or terminally ill)
All adult women who reported at the OPD of the UHTC participated in the study. They were briefed about it. They were divided into groups of 10–12 every day during the study period. For each batch, awareness sessions were taken by the PI regarding the measurement of their BP and its control by color coding approach, which included advice on diet, exercise, physical activity, and medication. First, a basic health assessment of the study population was done. This focused on basic socio-demographic data of the adult women, their health status, history of the present complaints, risk profile, treatment-seeking behavior, etc. After the concerned doctor noted, these details on a pro forma developed for this purpose. Thus, allowing the patients to relax for a while, the BP was measured in a sitting position by a mercury sphygmomanometer during routine clinic hours (0900–1400 h).
A modality of addressing the problem of HTN through the concept of spectrum approach was implemented. The patients received a color-coded BP record booklet.
We gifted colored plastic glasses (tumblers) to the patients so that interest was generated among them. Furthermore, this way, they would remember the color-coded segmentation. The corresponding color-coded areas are divided into five areas. The green area corresponded to a BP reading up to a maximum of 120/80 mmHg, the yellow area corresponded to a systolic blood pressure (SBP) reading over 120–129 mmHg, and diastolic blood pressure (DBP) reading <80 mmHg and any apparent HTN risk factors, like a positive family history. The blue color corresponded to a SBP reading, of 130– 139 mmHg and a DBP reading of < 89 mmHg and a clinical diagnosis of HTN by a physician. Orange color depicted SBP reading of 140 mmHg and more than 140 mmHg and DBP reading of more than 90 mmHg and some evidence of complications of HT. The red color corresponded to a SBP reading of more than 180 mmHg and more than 120 mmH g and History of any invasive procedure for complications of HT, for example, stent, pacemaker, kidney transplant, and dialysis.
Those who were given green glass were asked to stick to their usual routine and carry out daily physical activity; those with yellow glass were to follow lifestyle modification and keep a watch on their BP through regular monitoring; blue ones were to continue with regular physical/laboratory check-up, and treatment, along with lifestyle modification; orange ones were to follow strict adherence to medication along with lifestyle modification and salt reduction and consultation for invasive procedures; and red ones needed rehabilitation related to the invasive procedures and routine follow-up. We also distributed leaflets to our study subjects for awareness regarding HTN prevention and control.
Statistical analysis
Data entry and tabulation were done using Microsoft Excel. Percentage, mean, median, mode, range, and standard deviations were used to describe the data.
Ethical aspects
Permission of authorities and respondents’ consent was taken for the study. Approval was obtained from the Institutional Ethics Committee. Confidentiality of data was assured.
RESULTS
The majority of respondents were married (75.4%). Their literacy rate was 72% [Table 1]. The majority of the respondents were homemakers (58.2%). The mean age of the respondents was 38.23 years, (range 18–75 years).
| Socio-demographic profile | Categories | Frequency | Percentage |
|---|---|---|---|
| Marital status | Single | 34 | 13.3 |
| Married | 193 | 75.4 | |
| Divorced | 17 | 6.6 | |
| Widowed | 12 | 4.7 | |
| Education level | No formal education | 72 | 28.1 |
| Primary school | 60 | 23.4 | |
| Secondary school | 62 | 24.2 | |
| Higher secondary school | 31 | 12.1 | |
| College degree | 23 | 9.0 | |
| Postgraduate degree | 8 | 3.1 | |
| Occupation | Employed full time | 6 | 2.3 |
| Employed part-time | 8 | 3.1 | |
| Self-employed | 39 | 15.2 | |
| Unemployed | 39 | 15.2 | |
| Homemaker | 149 | 58.2 | |
| Student | 10 | 3.9 | |
| Retired | 5 | 2.0 |
Monthly household income ranged from Rs. 1,000 to 60,000, with a mean of Rs. 10,611.72. The average family size was 4.61 members.
Overall, 39.07% of the respondents reported being diagnosed with HTN, with 31% of them having been diagnosed for less than a year, 27% for 1–5 years, 23% for 5–10 years, and 19% for over 10 years. The mean systolic blood pressure (SBP) of the respondents was 127.64 mmHg, (range 80–190), while the mean diastolic blood pressure (DBP) was 80.19 mmHg (range 48–164). Most (78%) of them were currently taking medication for HTN. Some (34.4%) reported a family history of HTN; 5.50% mentioned being diagnosed with other chronic health conditions, including diabetes mellitus, hemiparesis, and thyroid issues [Table 2].
| Hypertension-related profile | Categories | Frequency | Percentage |
|---|---|---|---|
| Diagnosed with hypertension | Yes | 100 | 39.07 |
| No | 156 | 60.93 | |
| Time since diagnosed | Less than 1 year | 31 | 31.00 |
| 1–5 years | 27 | 27.00 | |
| 5–10 years | 23 | 23.00 | |
| More than 10 years | 19 | 19.00 | |
| Currently taking medication | Yes | 78 | 78.00 |
| No | 22 | 22.00 | |
| Family history | Yes | 88 | 34.40 |
| No | 133 | 52.00 | |
| Not sure | 35 | 13.60 | |
| Comorbidity | Asthma | 1 | 0.40 |
| Cataract | 1 | 0.40 | |
| Diabetes mellitus | 14 | 5.50 | |
| Gouty arthritis | 1 | 0.40 | |
| Hemiparesis | 3 | 1.20 | |
| Liver cirrhosis | 1 | 0.40 | |
| Migraine | 2 | 0.80 | |
| Nephrotic syndrome | 1 | 0.40 | |
| Stroke | 1 | 0.40 | |
| Thyroid | 2 | 0.80 | |
| None | 229 | 89.50 |
Table 3 shows the level of prevention-based color-coded stratification of the respondents. More than one-fifth (57) respondents were free of any evidence of HTN; 99 (39%) were at risk of developing HTN; 36(14%) diagnosed HTN cases were without any apparent complications, while 53(21%) had some complications. Eleven (4%) respondents needed rehabilitation.
| Level of prevention applicable | Color-coded stratification | Number | Percentage |
|---|---|---|---|
| Health promotion | Green | 57 | 22.2 |
| Specific protection | Blue | 99 | 38.7 |
| Early diagnosis/treatment | Yellow | 36 | 14.1 |
| Disability limitation | Orange | 53 | 20.7 |
| Rehabilitation | Red | 11 | 4.3 |
DISCUSSION
Uncontrolled BP is one of the main risk factors for cardiovascular disease (CVD) which are responsible for one-third of total deaths in India. The prevalence of HTN in adult men and women have been reported to be 30–35% globally.[11] In India also, it was 29–33%, that is, at least one in three adults has HTN.[12,13] In our study also, the point prevalence of HTN was 39% in women. Thus, our findings are in tandem with the scenario elsewhere in India. Almost one-third of them were recently diagnosed (<1 year). This indicated a consistent incidence of HTN in the community. One-fifth of them were chronic cases (>10 years since diagnosis).
Color coding is a systematic process of displaying information using different colors to assist in classification and identification. The Color coding system is used in many diagnostics and therapeutic modalities. Risk profiling through a color-coded client segmentation-based public health approach is useful in educating the community to deal with the problem of HTN and averting deaths due to acute hypertensive disorders.[5-10]
In low-income settings, the use of color coding in health systems has enhanced the quality of healthcare services by field workers, to classify ailments based on colors, diagnose the disease, start the appropriate treatment, and ensure better compliance. This endeavor has managed to improve existing poor health indicators. It also minimizes human errors in diagnosing and therapeutic modalities.
In our study, a level of prevention approach was applied simultaneously along with the color-coded stratification of the respondents. This involved the application of an individualized patient care approach by providing them with different colored cards on which HTN-related advice was written as per the level of prevention needed.
For example, green colored cards were provided to nonhypertensive participants whose SBP/DBP were normal. In this study, more than one-fifth (22%) of the respondents were eligible for being slotted in the health promotion segment; yellow colored cards were given to non-hypertensive participants with BP at borderline (SBP = 121139 mmHg and/or DBP = 8189 mmHg). Such respondents (39 %) were at risk, that is, to be put under specific protection (with a positive family history and obesity, etc.). Newly diagnosed patients were 14%; blue colored cards were given to these previously non-hypertensive participants with 1st time BP readings of SBP >140 mmHg/or DBP >90 mmHg. They advocated early diagnosis/treatment. One-fourth of the respondents with complications had HTN-related cardiological interventions such as stents. Disability limitation was applicable in 21% of the cases; orange cards were provided to such known hypertensive patients. Red cards were given to the survivors of HTN-related complications, who needed rehabilitation (4 %).
Limitations of the study
This was a small-scale study of 2 months only. It did not include the impact of the education given to the subjects who received training about the color coding-based client segmentation program for HTN control.
CONCLUSION
The present study successfully used the color coding-based client segmentation comprehensive care program for HTN control in a community setting of UHTC of a private medical college.
This involved the application of an individualized patient care approach by providing them with different colored cards on which HTN-related advice is written as per the level of prevention needed. Overall, 39% of the respondents had HTN. About two-fifths of respondents were at risk of developing HTN. This method has the potential to enhance the individualized management of HTN.
Acknowledgment
The authors acknowledge the financial support provided by the Prajjwalika scheme, WINCARS. Thanks are also due to the staff of the UHTC for their assistance in this research.
Ethical approval
The research/study was approved by the Institutional Review Board at SRMSIMS, Bareilly, UP, number SRMS IMS/ECC/2023/24, dated May 2, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Prajjwalika scheme, WINCARS.
References
- Trends in Hypertension Epidemiology in India. J Hum Hypertens. 2004;18:73-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular Mortality Associated with 5 Leading Risk Factors: National and State Preventable Fractions Estimated from Survey Data. Ann Intern Med. 2015;163:245-53.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence, Awareness, Treatment, and Control of Hypertension among the Elderly in Bangladesh and India: A Multicentre Study. Bull World Health Organ. 2001;79:490-500.
- [Google Scholar]
- Inaccurate Colour Coding of Medical Gas Cylinders. Anaesthesia. 2009;64:690.
- [CrossRef] [PubMed] [Google Scholar]
- Colour Coding, Drug Administration Error and the Systems Approach to Safety. Eur J Anaesth. 2007;24:385-6.
- [CrossRef] [PubMed] [Google Scholar]
- Risk Factors for Cardiovascular Disease among Adults in Rural Lucknow: A Community-based Study. Natl J Physiol Pharm Pharmacol. 2022;12:2020-5.
- [CrossRef] [Google Scholar]
- Colour Coding-based Client Segmentation Approach: A Neglected Yet Powerful Tool to Tackle non Communicable Diseases in High Burden and Low Resource Setting Countries-A Primary Care Approach. J Family Med Prim Care. 2020;9:5846-9.
- [CrossRef] [PubMed] [Google Scholar]
- Colour Coded Client Segmentation (CCCS) Public Health Approach to Educate the Community to Deal with Problem of Hypertension: A Pilot Study. J Educ Health Promot. 2021;10:41.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic Diseases and Injuries in India. Lancet. 2011;377:413-28.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetes and Hypertension in India: A Nationally Representative Study of 1.3 Million Adults. JAMA Intern Med. 2018;178:363-72.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertension Screening, Awareness, Treatment, and Control in India: A Nationally Representative Cross-sectional Study among Individuals Aged 15 to 49 Years. PLoS Med. 2019;16:e1002801.
- [CrossRef] [PubMed] [Google Scholar]








