Translate this page into:
Role of Neck Vessel Doppler in Correlation with Coronary CT Angiography for Assessing Coronary Artery Disease Burden in Diabetic Women and Men
*Corresponding author: Sankeerth Kendyala, Departemnt of Radiology and Imageology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India. sankeerth7498@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kendyala S, Yarlagadda J. Role of neck vessel Doppler in correlation with coronary CT angiography for assessing coronary artery disease burden in diabetic women and men. Indian J Cardiovasc Dis Women. 2023;8:235-44.
Abstract
Objectives:
With an incidence of 4.1 for women and 6.4 for men/1000 person-years, cardiovascular disease is the primary cause of morbidity and mortality for both men and women worldwide.[1] In asymptomatic patients, subclinical atherosclerosis has been detected utilising several non-invasive methods, such as computed tomography (CT) coronary angiography and Neck Vessel Doppler (NVD) to test coronary calcification. The goal of the present study was to assess the role of NVD in correlation with coronary CT angiography (CCTA) in assessing the coronary artery disease (CAD) burden in diabetic women and men patients.
Materials and Methods:
This study was conducted on 30 female patients and 30 male patients aged 40–60 years, who were referred for CCTA for suspected CAD at Nizam’s Institute of Medical Sciences Hospital, Hyderabad. This study was an observational and prospective study of diabetes mellitus patients. All subjects underwent NVD and CCTA scan on the same day. Carotid intimal media thickness (CIMT) was considered the largest of the two separate values (left and right CIMT). The analysis examined factors associated with coronary artery calcification defined as a coronary artery calcium (CAC) score >0.
Results:
The mean age at assessment was 52.6 years in the diabetic male group and 53.7 in the diabetic female group. 63% of the study population was also hypertensive in the male group and 77% of the study population was also hypertensive in the female group. Mean CIMT was 1.01 mm in the diabetic male group and 1.02 mm in the diabetic female group. Twenty-two (73.3%) patients in the diabetic male group had a CAC score >0, of which 4 (18.18%) had severe coronary artery calcification (CAC score >400 Au), 7 (31.81%) had moderate coronary artery calcification (CAC score 100–400 Au), 11 (50%) had mild coronary artery calcification (CAC score 1-99 Au), and 8 out of 30 (26.67%) had no coronary artery calcification (CAC score <0 Au). Twenty (66.67%) patients in the diabetic female group had a CAC score >0, of which 2 (10%) had severe coronary artery calcification (CAC score >400 Au), 7 (35%) had moderate coronary artery calcification (CAC score 100–400 Au), 11 (55%) had mild coronary artery calcification (CAC score 1-99Au) and 10 out of 30 (33.33%) had no coronary artery calcification (CAC score <0 Au). Mean CIMT and carotid plaque were significantly associated with CAC (P = 0.046 and P = 0.026, respectively, in the diabetic male’s group and P = 0.008 and P = 0.011, respectively, in the diabetic female’s group). The significance was more profound in the diabetic female group when compared to the diabetic male group.
Conclusion:
NVD giving various surrogate parameters such as CIMT and plaque, in correlation with CCTA (CAC score), can play a significant role in assessing the CAD burden in men and women with diabetes and hypertension, thereby helping the clinician to assess the future risk for stroke or myocardial ischemic events to take active interventions.
Keywords
Neck vessel Doppler
Calcium score
Carotid plaque
Coronary artery disease
Carotid intimal media thickness
Computed tomography
Coronary angiography
ABSTRACT IMAGE

INTRODUCTION
With an incidence of 4.1 for women and 6.4 for men/1000 person-years, cardiovascular disease is the primary cause of morbidity and mortality for both men and women worldwide.[1] In both industrialized and developing nations, diabetes mellitus (DM) is a significant cause of cardiovascular morbidity and mortality. At present, 382 million people are believed to have DM worldwide. By the year 2035, this number is expected to increase to 592 million.[2]
In comparison to the non-DM population, patients with DM typically have a greater degree of atherosclerosis, a higher incidence of multivessel coronary artery disease (CAD), frequent silent myocardial ischemia, and infarction with a higher risk of cardiac events.[3,4] Patients with DM continue to have a worse prognosis than non-DM patients after CAD develops clinically, both immediately following the incident and during long-term follow-up.[5]
In asymptomatic patients, subclinical atherosclerosis has been detected utilizing several non-invasive methods, such as computed tomography (CT) coronary angiography and Neck Vessel Doppler (NVD) to test coronary calcification. Since higher carotid intimal media thickness (CIMT) has been linked to a high prevalence of CAD and upcoming cardiovascular events,[4,6,7] it has been frequently utilized as a marker to diagnose subclinical atherosclerosis.[8,9]
The goal of the present study was to determine whether CIMT and carotid plaque can be used to identify diabetes patients who are at high risk for cardiovascular disease. Relationships between CIMT/carotid plaques and the existence and severity of coronary artery calcium (CAC) were investigated prospectively in diabetic patients undergoing non-invasive multi-slice CT. Coronary CT angiography (CCTA) shows the luminal and wall properties of the coronaries, such as the thickness of the plaque, the level of calcification, the degree of stenosis, and remodeling.[10]
Objective
The aim of the study was to assess the role of NVD in correlation with CCTA in assessing the CAD burden in diabetic women and men patients.
MATERIALS AND METHODS
This study was conducted on 30 female patients and 30 male patients aged 40–60 years, who were referred for CCTA for suspected CAD at Nizam’s Institute of Medical Sciences Hospital, Hyderabad. This study was an observational and prospective study of DM patients. All subjects underwent NVD and CCTA scan on the same day. A monthly average of 10 subjects (5 male and 5 female subjects) that matched the inclusion and exclusion criteria over a duration of 6 months were included in the study, amounting to a minimum of 60 participants (30 diabetic male and 30 diabetic female subjects) for the study.
Patients who were established Type II DM (T2DM) for ≥1 year, aged 40–60 years and with no history of CAD were included into the study. Pregnant women, patients with atrial fibrillation, and aged <40 years and >60 years were excluded from the study.
All patients included in the study gave written informed consent before enrolment.
Baseline demographic data were provided by all the patients. Clinical data were obtained with the patient’s informed consent and included sex, age, duration of DM, and hypertension history.
All patients who were referred to the department of radiology and imageology for evaluation of CAD underwent CT coronary angiogram using a 128-slice MDCT (Somatom Definition AS+/Siemens Healthcare Solutions, Germany) with scanning parameters of 120kV per tube energy with a current of 560 mA, 1 mm slice thickness, and a gantry rotation period of 200 ms. Images were obtained while breath-holding. The field of view was set from the carina to both domes of the diaphragm.
Necessary patient preparations like whether the serum creatinine level of the patients was within the normal range, a controlled heart rate of 65 bpm was maintained and other routine CT CAC parameters were checked before the scan.
While the CT scanning was being performed, the patients were asked to remain still. The image was acquired on breath holding for 10–25 s. A non-enhanced retrospective electrocardiogram-gated calcium-scoring study was performed. If the coronary calcium score values are ≥400, the patient was not a candidate for CT coronary angiogram and he/she was advised conventional angiogram for accurate evaluation.
The start of the reconstruction window for a single segment of the cardiac cycle was determined using the relative approach. The data set underwent image reconstruction at the two-time points of 30% R-R and 60% R-R.
An area of at least three “face-connected” voxels in the axial plane along the coronary arteries with an attenuation threshold of 130 HU or higher was defined as CAC. Calcium scores for each test were calculated by the software and expressed as Agatston scores of CT reference calcium scores. Each high-density lesion in the epicardial coronary artery was recorded and the sum of all identified lesions gave his CAC score for the entire coronary system, as reported by Agatston et al. The Agatston calcium (Au) score was calculated by an experienced single investigator blinded to clinical data to quantify the extent of CAC [Figure 1].

- Coronary artery calcium (CAC) scores: (a) CAC score of 714 Au (significantly increased risk) was calculated in a patient from the diabetic male group. (b) CAC score of 229.1 (moderate increased risk) Au was calculated in a patient from the diabetic female group.
CAC scores ranged from no increase (0 Au), mild increase (1–99 Au), moderate increase (100–400 Au), and significantly increased risk (>400 Au), depending on CHD risk.[11]
All patients who underwent CT CAC on that day also underwent NVD using a B-mode ultrasound system, using a high-resolution linear array transducer (4–12 Hz) in Esaote Mylab 9xp™. Intima-media thickness (IMT) was defined as the distance between the edge of the lumen-intima interface and the edge of the media-adventitia interface. On a longitudinal display, near and far walls were recognized as two bright lines separated by hypoechogenic space [Figure 2].

- Carotid intimal media thickness (CIMT): (a) CIMT of 0.7 mm was measured in a patient from the diabetic male group. (b) CIMT of 0.6 mm was measured in a patient from the diabetic female group.
The patient was examined in the supine position with the head slightly extended in the opposite direction of the carotid artery being examined. CIMT was measured at the far wall of the distal common carotid artery 1 cm proximal to the carotid bulb.
The entire carotid system was surveyed bilaterally for the presence of plaque [Figure 3]. The presence of carotid plaque was defined as a focal increase in thickness (>50%) of the rest of the vessel’s CIMT.[12] The ultrasound measurements were made by an experienced doctor who was blinded to CAC results.

- Carotid Plaque: (a) Carotid plaque noted in a patient from the diabetic male group. (b) Carotid plaque noted in a patient from the diabetic female group.
Statistical analysis
Analysis was performed using Microsoft excel. All categorical variables were expressed as percentages and continuous variables as mean (interquartile range). CIMT was considered the largest of the two separate values (left and right CIMT). The analysis examined factors associated with coronary artery calcification defined as a CAC score >0.
In addition to conventional risk factors for predicting coronary artery calcification, whether there are additional benefits of CIMT and carotid plaque were evaluated and investigated. Only two major risk factors were included to limit the number of variables in this analysis, indicating association bias in univariate analysis (P < 0.2).
A final series of analyses explored the results on a more detailed scale. Instead of simply the presence or absence of coronary artery calcification (defined as CAC >0), the CAC score was considered in four categories (0, 1–99, 100–400, and >400). Each risk factor was considered individually to examine the association between cardiac risk factors and this revised result.
P < 0.05 was used to indicate statistical significance.
Data were further compared between male and female diabetic patients.
RESULTS
The mean age at assessment was 52.6 years in the diabetic male group and 53.7 in the diabetic female group.
About 63% of the study population was also hypertensive in the male group and 77% of the study population was also hypertensive in the female group.
Both mean duration of diabetes, presence of hypertension and duration of hypertension was found to be slightly higher in the diabetic female group in comparison to the diabetic male group.
Mean CIMT was 1.01 mm in the diabetic male group and 1.02 mm in the diabetic female group. Not much significant difference can be noted between the two [Table 1].
| Diabetic males | Diabetic females | |
|---|---|---|
| Mean age | 52.6 years | 53.7 years |
| Duration of diabetes | 7.93 years | 8.3 years |
| Duration of hypertension | 4.03 years | 4.46 years |
| CAC | ||
| <0 | 8 | 10 |
| 0–100 | 11 | 11 |
| 100–400 | 7 | 7 |
| >400 | 4 | 2 |
| Mean CIMT | 1.01 mm | 1.02 mm |
CAC: Coronary artery calcium, CIMT: Carotid intimal media thickness
Twenty-two (73.3%) patients in the diabetic male group had a CAC score >0, of which 4 (18.18%) had severe coronary artery calcification (CAC score >400 Au), 7(31.81%) had moderate coronary artery calcification (CAC score 100–400 Au), 11 (50%) had mild coronary artery calcification (CAC score 1-99 Au), and 8 out of 30 (26.67%) had no coronary artery calcification (CAC score <0 Au).
Twenty (66.67%) patients in the diabetic female group had a CAC score >0, of which 2 (10%) had severe coronary artery calcification (CAC score >400 Au), 7 (35%) had moderate coronary artery calcification (CAC score 100–400 Au), 11 (55%) had mild coronary artery calcification (CAC score 1-99 Au) and 10 out of 30 (33.33%) had no coronary artery calcification (CAC score <0 Au) [Chart 1].

- Categorical comparison of calcium score in both diabetic male and diabetic female group.
The number of subjects with severe coronary calcification was found to be higher in the diabetic male group. The overall number of subjects with a CAC score >0 was more in the diabetic male group.
Individual associations between each risk factor and CAC score >0 were initially examined in a series of univariable analyses [Table 2].
| Variable | Category | CAC >0 | OR (95%CI) | P-value | |||
|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | ||
| Age | 41–45 years | 3/5 | 0/1 | 0.47 (0.06–3.53) | 0.15 (0.005–4.15) | 0.46 | 0.26 |
| 46–50 years | 2/4 | 5/8 | 0.3 (0.03–2.60) | 0.78 (0.14–4.21) | 0.27 | 0.77 | |
| 51–55 years | 6/9 | 6/8 | 0.62 (0.11–3.46) | 1.71 (0.27–10.58) | 0.59 | 0.56 | |
| 56–60 years | 11/12 | 9/13 | 7 (0.73–66.80) | 1.22 (0.26–5.73) | 0.09 | 0.79 | |
| Sex | Male | 22/30 | 1.3750 (0.4534–4.1703) | 0.5737 | |||
| Female | 20/30 | ||||||
| Hypertension | Present | 13/19 | 16/19 | 0.48 (0.08–2.95) | 9.33 (1.63–53.20) | 0.43 | 0.01 |
| Absent | 9/11 | 4/11 | |||||
| Duration of diabetes | >5 years | 16/20 | 18/24 | 2.67 (0.50–14.21) | 6.00 (0.87–41.44) | 0.25 | 0.07 |
| <5 years | 6/10 | 2/6 | |||||
| CIMT | Raised | 15/17 | 14/15 | 6.4 (1.02–40.26) | 21 (2.15–204.62) | 0.046 | 0.008 |
| Normal | 7/13 | 6/15 | |||||
| Plaque | Present | 14/14 | 14/14 | 29 (1.48–568.23) | 46.84 (2.37–926.11) | 0.026 | 0.011 |
| Absent | 8/16 | 6/16 | |||||
CAC: Coronary artery calcium, CIMT: Carotid intimal media thickness, OR: Odds ratio, CI: Confidence interval
Mean CIMT and carotid plaque were significantly associated with CAC (P = 0.046 and P = 0.26, respectively, in the diabetic male’s group and P = 0.008 and P = 0.011, respectively, in the diabetic female’s group). The significance was more profound in the diabetic female group when compared to the diabetic male group.
The presence of hypertension also showed a significant positive association in the diabetic female group when compared to the diabetic male group, where a significant association could not be established.
No other significant association could be derived from our data set in terms of age, sex, and duration of diabetes (P > 0.05).
Of the 22 subjects in the diabetic male group with a CAC score >0, 14 (63%) had a concomitant carotid plaque. All four patients with severe calcification and all seven patients with moderate calcification were associated with the prevalence of a carotid plaque. Only three patients out of 11 with mild calcification showed the presence of concomitant carotid plaque. Eight patients with a CAC score <0 showed no carotid plaque [Table 3].
| Number | Plaque | Raised CIMT | ||||
|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | |
| CAC <0 Au | 8 | 10 | 0 | 0 | 2 | 1 |
| CAC 0−100 Au | 11 | 11 | 3 | 5 | 4 | 6 |
| CAC100−400 Au | 7 | 7 | 7 | 7 | 7 | 6 |
| CAC >400 Au | 4 | 2 | 4 | 2 | 4 | 2 |
| Total | 30 | 30 | 14 | 14 | 17 | 15 |
CAC: Coronary artery calcium, CIMT: Carotid intimal media thickness
Of the 20 subjects in the diabetic female group with a CAC score >0, 14 (70%) also had a concomitant carotid plaque. Both patients with severe calcification and all seven patients with moderate calcification were associated with the prevalence of a carotid plaque. Five patients out of 11 with mild calcification showed the presence of concomitant carotid plaque. Ten patients with a CAC score <0 showed no carotid plaque [Chart 2].
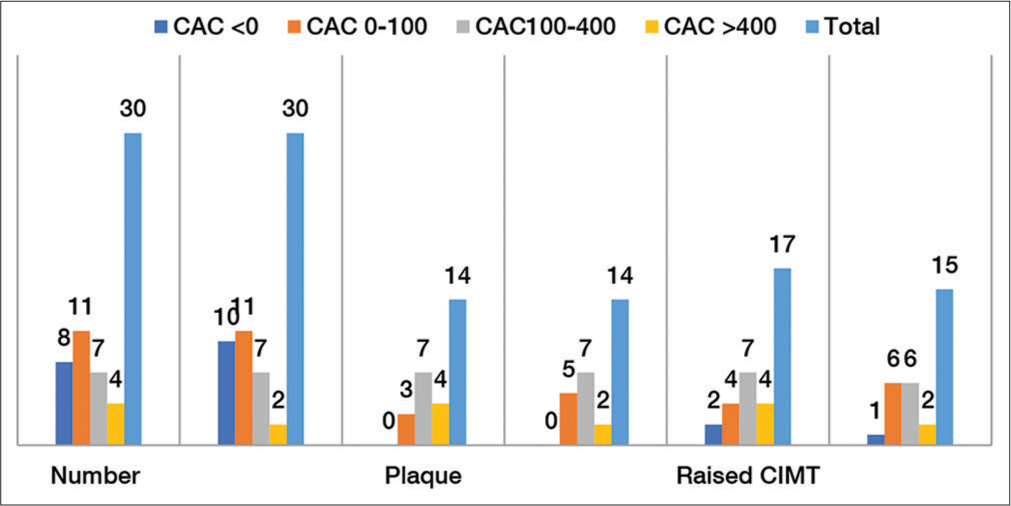
- Categorical comparison of calcium score with carotid plaque and raised carotid intimal media thickness in both diabetic male and diabetic female group.
On further analyzing the relation of the carotid plaque with the categorical division of CAC scores [Table 4], a CAC score of <0 showed a strong negative correlation, reinstating that patients with a carotid plaque were associated with CAC score >0, but not with a CAC score <0 in both the groups (P = 0.026, in the diabetic male’s group and P = 0.011, in the diabetic female’s group). A positive correlation was established with a CAC score of 100–400 Au and carotid plaque with P = 0.0219 in both groups (P < 0.05). No other significant correlation could not be derived from the categorical data. The significance was more profound in the female group.
| Plaque+ | OR (95%CI) | -value | ||||
|---|---|---|---|---|---|---|
| M | F | M | F | M | F | |
| CAC <0 | ||||||
| Y | 0/8 | 0/10 | 0.03 (0.002−0.675) | 0.0213 (0.001−0.422) | 0.0265 | 0.0115 |
| N | 14/22 | 14/20 | ||||
| CAC 0−100 | ||||||
| Y | 3/11 | 5/11 | 0.2727 (0.054−1.363) | 0.926 (0.209−4.11) | 0.1136 | 0.9194 |
| N | 11/19 | 9/19 | ||||
| CAC 100−400 | ||||||
| Y | 7/7 | 7/7 | 33 (1.66−656.27) | 33 (1.66−656.27) | 0.0219 | 0.0219 |
| N | 7/23 | 7/23 | ||||
| CAC 100−400 | ||||||
| Y | 4/4 | 2/2 | 14.1429 (0.69−290.53) | 6.6 (0.29−150.1) | 0.0858 | 0.2369 |
| N | 10/26 | 12/28 | ||||
CAC: Coronary artery calcium, OR: Odds ratio, CI: Confidence interval
Similarly, on further probing the relation of raised CIMT with the categorical division of CAC scores [Table 5], it was found that a strong negative correlation was established with CAC score <0 and raised CIMT. This validated that the above-derived correlation of patients with raised CIMT was associated with CAC score >0 but not CAC score <0 (P = 0.0468, in the diabetic male group and P = 0.0088, in the diabetic female group). No other significant association could be derived from the categorical data set; however, CAC score 100–400 Au group was close to establish an association with P values just over 0.05 (P = 0.0511, in the diabetic male’s group and P = 0.0545, in the diabetic female’s group).
| Raised CIMT | OR (95%CI) | P-value | |||||
|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | ||
| CAC <0 | |||||||
| Y | 2/8 | 1/10 | 0.15 (0.025−0.974) | 0.0476 (0.005−0.464) | 0.0468 | 0.0088 | |
| N | 15/22 | 14/20 | |||||
| CAC 0−100 | |||||||
| Y | 4/11 | 611 | 0.26 (0.055−1.26) | 1.33 (0.3−5.9) | 0.0948 | 0.7051 | |
| N | 13/19 | 9/19 | |||||
| CAC 100−400 | |||||||
| Y | 7/7 | 6/7 | 19.3 (0.98−377.5) | 9.33 (0.96−90.94) | 0.0511 | 0.0545 | |
| N | 10/23 | 7/23 | |||||
| CAC >400 | |||||||
| Y | 4/4 | 2/2 | 9 (0.44−183.98) | 5.74 (0.25−130.38) | 0.1535 | 0.2727 | |
| N | 13/26 | 13/28 | |||||
CAC: Coronary artery calcium, CIMT: Carotid intimal media thickness, OR: Odds ratio, CI: Confidence interval
DISCUSSION
Our study found that coronary artery calcifications are common in T2DM patients. Our analysis revealed strong positive associations of coronary calcification with a carotid plaque and raised CIMT.
A study was conducted on the residents of Muscatine, Iowa, in 1999, by Davis et al.,[13] titled “Increased carotid intimal thickness and coronary calcification are related in young and middle-aged adults – The Muscatine Study.” All the subjects aged between 33 and 42 years and included 182 men and 136 women. Statistical average of twelve measurements of maximal carotid IMT was determined by B-mode ultrasonography of carotid vessels. Mean IMT was 0.788 mm (Standard deviation [SD] 0.127) in men and 0.720 mm (SD 0.105) in women. Nearly one-fourth of men (27%) and nearly three 20ths of women showed CAC and it showed significant association with IMT in men (P < 0.025) and women (P < 0.005). An association in young adults was established between raised carotid IMT and CAC and between cardiovascular risk factors and increased IMT. It was concluded that premature atherosclerosis in young adults could be identified using coronary artery calcifications as well as carotid intimal media thickness.
Our study with a sample size of 30 diabetic males and 30 diabetic females, aged between 40 and 60 years, showed a mean CIMT of 1.01 mm in the male group and 1.02 mm in the female group. CAC was present in 73.33% of men and 66.66% of women in the study sample and was significantly associated with IMT in men (P < 0.05) and women (P < 0.01). It mirrored that a strong association is present between CIMT and CAC, thereby aiding in assessing the CAD burden.
Kablak-Ziembicka et al.[14] conducted a study which was published in issue 11, volume 90 of the BMJ in 2004, titled “Association of increased carotid IMT with the extent of coronary artery disease.” Five hundred and fifty-eight consecutive patients (438 men) underwent CT coronary angiography and carotid ultrasonography, with a mean (SD) age of 58.8 (9.2) years. A profound increase in IMT was observed in patients with one, two, and three vessels. Patients were 94% likely to have CAD when a log-normal distribution of IMT values showed that if the mean IMT was >1.15 mm (sensitivity of 65% and specificity of 80%) in patients at high risk of CAD. A positive correlation between increasing IMT and advanced CAD was detected by coronary angiography in their study with a sample size of 558 patients with suspected CAD. This study also throws light on the role of IMT is not just restricted for CAD screening, as well as to detect the extent of the disease.
Our study was in concordance with Kablak-Ziembicka et al., raised CIMT was noted in 68.18% of the CAC score >0 diabetic male group and 70 % of the CAC score >0 diabetic female group. This suggests that the presence of raised CIMT increases the probability of CAD.
Oei et al.[15] published their research in the Journal of the American College of Cardiology, 2002, titled “Association between electron beam CT -assessed coronary calcification and measures of extra-coronary atherosclerosis: The Rotterdam Coronary Calcification Study” which studied 2013 patients aged 55 years and older. Electron beam CT scan was performed on all participants and Agatston calcium score was used to quantify Coronary calcification. Measures of extracoronary atherosclerosis included common carotid IMT, carotid plaque, ankle-arm index (AAI), and aortic calcification. Associations were strongest for carotid plaques and aortic calcification; coronary calcification increased from the lowest category (no plaques) to the highest category 9 times and 11 times in men and 10 times and 20 times in women, respectively.
Our study paralleled with Oei et al., where 63.63% and 70% of diabetic male and female groups, respectively, showed the presence of carotid plaque in CAC scores>0, with a significant association of plaque with CAC scores. This also paves the way to establish atherosclerosis in other systemic vessels.
Nambi et al.,[6] in their study published in the Journal of the American College of Cardiology, 2011, titled, “Carotid IMT and presence or absence of plaque improves prediction of coronary heart disease risk in the Atherosclerosis Risk in Communities (ARIC) study” exhibited that by adding CIMT measurement and carotid plaque information to the traditional risk factors (TRF), CAD prediction could be remarkably improved. TRF-only, TRF + C-IMT, TRF + plaque, and TRF + C-IMT + plaque were included after considering risk prediction models. On a sample of 13,145 eligible subjects (5682 men and 7463 women), the model predictivity was estimated by calculating the area under the receiver operating characteristic curve (AUC). Overall, the AUC increased for the TRF-only, TRF + C-IMT, TRF + plaque, and TRF + C-IMT + plaque model, respectively, with the addition of C-IMT and plaque separately or together to the TRF model.
Like our study significant associations were established in a study conducted by Nanbi et al., it can be reflected that both CIMT and carotid plaque are great surrogate parameters to assess CAD burden. Most conventional risk-stratifying logarithms like Framingham and QRISK do not include these parameters in their criteria. Further research is needed to substantiate that the addition of these parameters to the existing logarithms will provide additional substantial benefits.
Cohen et al.[16] conducted a study published in JACC: Cardiovascular imaging in 2013, titled, “Relationship between carotid artery disease by ultrasound and CAD by coronary CT angiography” to study the relationship and identify carotid ultrasound parameters predictive of CAD. The sample of 150 subjects who were referred for CT angiography (CTA) underwent carotid ultrasonography on the same day. Nearly half of subjects with a calcium score of 0 (30 of 63) showed the presence of carotid plaque and in almost nine-tenths of subjects with a calcium score >0 (77 of 87) showed the presence of carotid plaque (P = 0.0001). Significant association was established between calcium score >0 (odds ratio [OR]: 5.4, P < 0.0001, 2.7, P < 0.001; 2.9, P = 0.011, respectively) and disease in at least one vessel on CTA (OR: 2.8, P = 0.03, 2.19, P = 0.073; 2.22, P = 0.058, respectively) with carotid plaque, IMT ≥1.5 mm, or mean IMT diameter >0.75 mm, respectively. A conclusion was derived that the presence and severity of coronary calcification and disease on CTA in ambulatory subjects were associated with both carotid plaque and increased carotid IMT.
Our study showed that carotid plaque was present in 14 out of 30 patients in both the diabetic male and female groups. It was present in 63.63% and 70% of diabetic male and female groups, respectively, with CAC score >0. The OR of 29 and 46.84 was seen in the diabetic male and female groups, respectively, with P = 0.026 and 0.011. It was showing a strong positive association like the study conducted by Cohen et al. This also correlated the association of carotid plaque and increased carotid IMT with the presence and severity of coronary calcification and disease on CTA noted in their study.
A prospective study was conducted in 2017 on a cohort of 262 asymptomatic patients with T2DM entitled “Relation between carotid atherosclerosis and coronary artery calcification in asymptomatic diabetic subjects – a prospective multicenter study” by Jeevarethinam et al.,[17] using carotid ultrasonography to evaluate CIMT and carotid plaque and CT-CAC CT. Mean CIMT was 0.75 ± 0.14 mm and nearly half of the participants showed carotid plaque. CAC score >0 was present in three fourths of the population, severe coronary atherosclerosis (>400 Au) was present in one fifths of them. 40 (70%) patients (P < 0.001) showed the presence of carotid plaque. Profound associations were established between non-zero CAC score and age (P < 0.001), hypertension (P = 0.01), gender (P = 0.003) and duration of diabetes (P = 0.004) via univariable analysis. Nonzero CAC score was remarkably associated with carotid plaque and mean CIMT (ORs [95% confidence interval, CI], 3.12 [1.66– 5.85] and 2.98 [0.24–7.17], respectively order).
Our study mirrored the study conducted by Jeevarethinam et al. The number of subjects with CAC scores>0 comprised 22 (73.4%) and 20 (66.67%) in diabetic male and female groups, respectively. Four (18.18%) patients had severe coronary artery calcification out of 22 patients (CAC score >0) in diabetic male group and 2 (10%) patients had severe coronary artery calcification out of 20 patients (CAC score >0) in diabetic female group. Plaques were present in all patients (100%) with severe coronary artery calcification (CAC score >400). Carotid plaque and CIMT showed significant association with CAC score >0 (odd’s ratios [95% CI] 6.4 (1.02–40.26) and 21 (2.15–204.62) for CIMT in diabetic male and female group, respectively, and 29 (1.48–568.23) and 46.84 (2.37–926.11) for Carotid plaque in diabetic male and female group, respectively. Both studies concurred that carotid plaque and CIMT are predictive indicators for CAD.
However, our findings were not consistent with a nested case–control study by Del Sol et al.[18] titled “Is carotid intimal thickness useful in assessing cardiovascular disease risk? The Rotterdam Study Stroke.” The sample population belonged to 55 years and older and had participated in the Rotterdam Study. They constituted 374 subjects with either stroke or myocardial infarction as cases and 1496 controls. The predictive value of the identified risk factors and the added value of IMT were estimated by logistic regression modeling and the area under the receiver operating characteristic curve (ROC area). 0.65 was the ROC area of the model with only age and gender (95% CI, 0.62–0.69). Independent risk factors(previous myocardial infarction and stroke, DM, smoking, systolic blood pressure, diastolic blood pressure, and total and high-density lipoprotein cholesterol levels) increased the ROC area from 0.65 to 0.72 (95% CI, 0.69–0.75). Among all subjects with coronary heart disease and cerebrovascular disease, this model accurately predicted 17%. The ROC area increased to 0.75 (95% CI, 0.72–0.78) by adding common carotid IMT to the previous model. The ROC area was 0.71 (95% CI, 0.68–0.74), and 14% of all subjects were accurately predicted, using only the IMT measure. It was derived that no substantial increase in predictive value was noted by adding IMT to the risk function of coronary heart disease and cerebrovascular disease.
Unlike their study, the 95% CI values for CIMT (1.02–40.26 in the diabetic male group and 2.15–204.62 in the diabetic female group) and carotid plaque (1.48–568.23 in the diabetic male group and 2.37–926.11 in the diabetic female group) showed very strong association in our study. These can be reliable markers of screening for CAD burden.
Limitations
As this study population was relatively small and observational, the validity of any of the conclusions offered needs to be tested in a larger population before any revision of guidelines can be recommended.
The study was conducted on patients referred for CCTA for suspected CAD, creating a referral bias and a higher number of subjects with suspected CAD. Whether the results of the study can stand true for asymptomatic patients needs to be evaluated.
The role of drugs such as anti-hypertensives, vasodilators, hypoglycemic drugs, and insulin were not considered for this study. Other confounding factors such as smoking, hyperlipidemia, and obesity which are high-risk causative factors were also not analyzed in our study.
The study was conducted in subjects aged 40-60, however in view of the rising trend of young MI and premature atherosclerosis,similar study can be conducted in younger populations to assess disease burden of CAD.
CONCLUSION
This study supports that non invasive investigation, NVD can be used as screening modality for assesing the CAD disease burden in high risk diabetic women and men. Neck Vessel Doppler giving various surrogate parameters such as CIMT and plaque, in correlation with CCTA (CAC score), can play a significant role in assessing the CAD burden in men and women with diabetes and hypertension, thereby helping the clinician to assess the future risk for stroke or myocardial ischemic events to take active interventions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Audio summary available at:
Financial support and sponsorship
Nil.
References
- Variations between women and men in risk factors, treatments, cardiovascular disease incidence, and death in 27 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet. 2020;396:97-109.
- [CrossRef] [PubMed] [Google Scholar]
- Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137-49.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality from coronary heart disease in subjects with Type 2 diabetes and nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229-34.
- [CrossRef] [PubMed] [Google Scholar]
- Risk stratification in uncomplicated Type 2 diabetes: Prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J. 2006;27:713-21.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular events in Type 2 diabetes: Comparison with non-diabetic individuals without and with prior cardiovascular disease. 10-year follow-up of the Hoorn Study. Eur Heart J. 2003;24:1406-13.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: The ARIC (Atherosclerosis Risk in Communities) study. J Am Coll Cardiol. 2010;55:1600-7.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: A segment-based comparison with intravascular ultrasound. Circulation. 2004;109:14-7.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid intima-media thickness as a biomarker of subclinical atherosclerosis. Swiss Med Wkly. 2012;142:w13705.
- [CrossRef] [Google Scholar]
- Common carotid intima-media thickness as a risk factor for outcomes in Asian patients with acute ST-elevation myocardial infarction. Can J Cardiol. 2014;30:1620-6.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of coronary plaque characteristics with coronary computed tomography angiography in patients with non-obstructive coronary artery disease: A long-term follow-up study. Eur Heart J Cardiovasc Imaging. 2016;18:1170-78.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic role of coronary calcium scoring in the rapid access chest pain clinic: Prospective evaluation of NICE guidance. Eur Heart J Cardiovasc Imaging. 2014;15:886-92.
- [CrossRef] [PubMed] [Google Scholar]
- Mannheim carotid intima-media thickness consensus (2004-2006). An update on behalf of the advisory board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004 and Brussels, Belgium, 2006. Cerebrovasc Dis. 2007;23:75-80.
- [CrossRef] [PubMed] [Google Scholar]
- Increased carotid intimal-medial thickness and coronary calcification are related in young and middle-aged adults. The Muscatine study. Circulation. 1999;100:838-42.
- [CrossRef] [PubMed] [Google Scholar]
- Association of increased carotid intima-media thickness with the extent of coronary artery disease. Heart. 2004;90:1286-90.
- [CrossRef] [PubMed] [Google Scholar]
- The association between coronary calcification assessed by electron beam computed tomography and measures of extra coronary atherosclerosis: The Rotterdam Coronary Calcification Study. J Am Coll Cardiol. 2002;39:1745-51.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between carotid disease on ultrasound and coronary disease on CT angiography. JACC Cardiovasc Imaging. 2013;6:1160-7.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between carotid atherosclerosis and coronary artery calcification in asymptomatic diabetic patients: A prospective multicenter study. Clin Cardiol. 2017;40:752-8.
- [CrossRef] [PubMed] [Google Scholar]
- Is carotid intima-media thickness useful in cardiovascular disease risk assessment? The Rotterdam Study. Stroke. 2001;32:1532-8.
- [CrossRef] [PubMed] [Google Scholar]







