Translate this page into:
Bending Saturation Index – A Novel Index of Old Symptom a Marker of Elevated Filling Pressure in Heart Failure
*Corresponding author: Purushotham Reddy, Department of Cardiology, Nizams Institute of Medical Sciences, Hyderabad, Telangana, India. purushotham3193@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Reddy P. Bending saturation index – A novel index of old symptom a marker of elevated filling pressure in heart failure. Indian J Cardiovasc Dis Women 2023;8:116-20.
Abstract
Objectives:
Bendopnea is a symptom in patients with heart failure (HF) defined as shortness of breath when bending forward. It is mediated by increased ventricular filling pressure during bending forward. Qualification of bendopnea and its correltion with other symptoms and parameters of HF is not a much explored area. In this study, we studied the frequency of bendopnea in patients admitted with HF and a index of difference between sitting and bending saturations and its correlation with clinical, laboratory, and echocardiographic and short-term mortality.
Material and Methods:
We conducted a study of 150 patients admitted with DHF in the span of 5 month and followed for 1 month. Bendopnea is defined as subjective sensation of worsening shortness of breath after bending for 1 min or more. Saturations after bending for 1 min are also recorded for each patient. Bendopnea saturation index (BOSI) is calculated as difference between saturations at baseline and after bending over, its percentage over baseline saturation (SaO2 sitting - SaO2 bending/SaO2 sitting*100).
Results:
It was present in 61 patients (40.7%). Among 150 patients, 11 patientns (7.3%) expired. Orthopnea was more frequent in patients with bendopnea compared to patients without (59% of patients with bendopnea also had orthopnea and 34.8% of patients without bendopnea had orthopnea, and the difference was statistically significant (P = 0.03). Paroxysmal nocturnal dyspnea (PND) was present in 29.5% of patients with bendopnea and 11% of patients without bendopnea (P = 0.05). The patients with bendopnea had higher right ventricular systolic pressure (RVSP) (49.9 ± 1.6) compared to patients without bendopnea (33.5 ± 0.9). Average NT pro BNP values were 8717 ± 950 pg/mL in patients with bendopnea and 1110 ± 99 pg/mL in patients without bendopnea (P < 0.005). Mean BOSI was 4.4 (±2.9) in patients with bendopnea and 0.4 (±0.09) in patients without bendopnea. There was a negative correlation between BOSI and left ventricular ejection fraction (LVEF), and positive correlation between BOSI and RVSP. Among patients with bendopnea, six patients expired, when compared with patients who were alive after 1 month using t-test, patients who expired have higher average BOSI (P < 0.005).
Conclusion:
Bendopnea and falling of desaturation on bending is a sign of significance in HF patients. The presence of bendopnea correlated with increased pulmonary arterial pressure and with other symptoms of respiratory variation, namely – orthopnea and PND, and higher values of biomarker (NTproBNP). BOSI, but not bendopnea had significant positive correlation with RVSP, and negative correlation with LVEF. BOSI also correlated with short-term mortality.
Keywords
Bendopnea
Bendopnea saturation index
Orthopnea
Paroxysmal nocturnal dyspnea
ABSTRACT IMAGE

INTRODUCTION
Since the first description of heart failure (HF), several respiratory symptoms related to the position (orthopnea and paroxysmal nocturnal dyspnea [PND]) have been described. These symptoms are used to classify HF according to NewYork Heart Association (NYHA). Bendopnea is a recently described symptom of HF where a patient will experience shortness of breath on bending forward while wearing shoes or tying laces.[1,2] Bendopnea is mediated by increased ventricular filling pressure on bending forward, which exacerbates already increased filling pressure in HF patients. It is also associated with the worse cardiac index, pulmonary capillary wedge pressure, and pulmonary artery pressure.[1] Furthermore, postural changes in HF patients may affect the bronchial vasculature and alter the airway caliber.[3] Recent studies have shown that bendopnea is associated with adverse outcomes of HF, and bendopnea has been associated with the severity of HF.[4,5] However, quantification of fall in saturation – bending oxygen saturation index Bendopnea saturation index (BOSI) and its correlation with other symptoms, biomarkers, and outcomes has not been studied much. We, in this study, have assessed the frequency of bendopnea along with other symptoms in patients admitted with decompensated HF.
Aims and objectives
The objectives of the study are as follows:
Assessing patients admitted with HF for the presence of worsening shortness of breath on bending forward (bendopnea)
Assessing saturations in sitting and bending positions and calculating the difference of saturations
Comparing with other symptoms of HF, echocardiographic parameters, and short-term mortality.
MATERIALS AND METHODS
We evaluated a total number of 150 patients with decompensated HF with both preserved and reduced ejection fraction, admitted to our hospital over a span of 5 months, from July 2022 to 2022.
Demographic data, symptoms at presentation (orthopnea, PND, abdominal fullness, and pedal edema), and echo parameters (Ejection fraction and right ventricular systolic pressure [RVSP]) are collected at presentation.
Patients in hypotension, patients on inotropes, altered sensorium, and morbidly obese patients were excluded from the study. Patients who were unable to bend forward for reasons not related to HF, as well as patients who experienced headaches or syncope on bending forward, were excluded from the study.
After informed consent, patients are asked to sit on a chair comfortably. Room air saturations of each patient are measured with a standard pulse oximeter, then patients are asked to bend forward and touch their ankles for a span of 1 min, during which time patients are asked whether or not they are experiencing any worsening shortness of breath. Bendopnea is defined as a subjective sensation of worsening shortness of breath after bending for 1 min or more. Saturations after bending for 1 min are also recorded for each patient. BOSI is calculated as the difference between saturations at baseline and after bending over, its percentage over baseline saturation (SaO2 sitting - SaO2 bending/SaO2 sitting*100). They were told to stop the maneuver when palpitations, headaches, or general malaise occurred. For patients who were admitted more than once, only the first admission was recorded. Death during the hospital admission or over a span of 1-month follow-up is considered and compared presence or absence of bendopnea and BOSI.
Normally distributed continuous variables were expressed as mean ± standard deviation. Categorical variables were expressed as numbers and percentages. We analyzed normally distributed continuous variables by Student’s t-test, proportions by χ2 test, and continuous variables with skewed distribution by Mann– Whitney test. The association between two continuous variables was assessed by Pearson correlation. The P-values for all tests were two-sided, and statistical significance was set at P ≤ 0.05.
RESULTS
Demographic data
Among 150 patients assessed, 61 (40.7%) had bendopnea. The mean age of the population is 55.5 (± 9.1). among the 150 patients, 76 (50.7%) were female and 74 (49.3%) were male. A total of 67 (44.7%) patients had orthopnea, 28 (18.7%) had PND, 9 (6%) had abdominal distention, and 73 (48.7%) had pedal edema. A total of 11 (7.3%) patients expired in the study group.
Mean saturation was 95% (± 2.9) in the sitting position, and 93% (± 4.1) in the bending position. [Table 1] includes bendopnea and its association with other clinical and laboratory parameters.
| With bendopnea (n=61) | Without bendopnea (n=89) | P-value | |
|---|---|---|---|
| Age | 56±1.7 | 55±1 | Not significant |
| Gender (male/female) | 27/34 | 47/42 | Not significant |
| Body mass index | 28.5±7 | 26.8±5.2 | Not significant |
| Mean saturations | 95±3.2% | 95±2.6% | Not significant |
| Orthopnea | 59% (36/61) | 34.8% (31/89) | P=0.03 |
| Paroxysmal nocturnal dyspnea | 29.5% (18/61) | 11.2% (10/89) | P=0.05 |
| Abdominal fullness | 8.2% (5/61) | 4.5% (4/89) | Not significant |
| Pedal edema | 45.9% (28/61) | 50.6% (45/89) | P=0.5 (NS) |
| Mean Bendopnea saturation index | 4.4±2.9 | 0.4±0.09 | P<0.005 |
| NT pro BNP (pg/mL) | 8717±950 | 1110±99 | P<0.005 |
| Mortality | 9.8% (6/61) | 5.6% (5/89) | P=0.3 (NS) |
An almost equal number of male and female patients were taken into the study. Twenty-seven among 61 (44%) patients with bendopnea were female. Bendopnea was not shown to have significant gender differences. However, since this is a smaller study, the association cannot be ruled out and a larger population has to be studied to see such an association.
The studied pathological backgrounds (hypertension, diabetes, atrial fibrillation, chronic obstructive pulmonary disease, and chronic kidney disease) showed no statistically significant difference between the two groups.
There was no significant difference between mean baseline saturations in sitting positions between the two groups.
Clinical parameters are shown in [Table 1].
Orthopnea was the most frequent symptom analyzed apart from shortness of breath in patients with HF. Orthopnea was more frequent in patients with bendopnea compared to patients without (59% of patients with bendopnea also had orthopnea and 34.8% of patients without bendopnea had orthopnea, and the difference was statistically significant (P = 0.03). PND was present in 29.5% of patients with bendopnea and 11% of patients without bendopnea and the difference was statistically significant (P = 0.05).
The frequency of abdominal fullness and pedal edema was not significantly different.
Mean BOSI was 4.4 (± 2.9) in patients with bendopnea and 0.4 (± 0.09) in patients without bendopnea. This difference was statistically significant (P < 0.005).
Average NT pro-BNP values were 8717 ± 950 pg/mL in patients with bendopnea and 1110 ± 99 pg/mL in patients without bendopnea. The difference between the two groups was statistically significant (P < 0.005).
There was no statistically significant difference between the two groups in comparing short-term mortality/outcome.
All the patients included in the study underwent transthoracic echocardiography and the parameters of interest were left ventricular ejection fraction (LVEF) and RVSP (which is similar to pulmonary artery systolic pressure [PASP]). These parameters are mentioned in [Table 2].
| With bendopnea | Without bendopnea | P-value | |
|---|---|---|---|
| LVEF (%) | 46.01±1.0 | 47.8±0.8 | P=0.16 |
| RVSP (mmHg) | 49.9±1.6 | 33.5±0.9 | P<0.0005 |
LVEF: Left ventricular ejection fraction, RVSP: Right ventricular systolic pressure
The mean LVEF of patients with bendopnea was 46.01 ± 1.0%, whereas that of patients without bendopnea was 47.8 ± 0.8. However, the difference was not statistically significant.
There was a significant difference (P < 0.0005) between mean RVSP values in the two groups. The patients with bendopnea had higher RVSP with a mean of 49.9 ± 1.6 compared to patients without bendopnea who had a mean RVSP of 33.5 ± 0.9.
Within the group of patients with bendopnea, a subgroup comparison was done to see the correlation between BOSI and short-term mortality, the results are shown in [Table 3].
| Patients alive | Patients expired | P-value | |
|---|---|---|---|
| Average BOSI | 3.9±2 | 8.4±1.1 | P<0.005 |
BOSI: Bendopnea saturation index
Among 61 patients with bendopnea, six patients expired, when compared with patients who were alive after 1 month, using t-test, patients who expired have higher average BOSI and the difference is statistically significant (P < 0.005).
Correlation between BOSI and LVEF and between BOSI and RVSP is done using the Pearson correlation graph as shown in [Figures 1 and 2].

- BOSI versus LVEF in patients with bendopnea. BOSI: Bendopnea saturation index, LVEF: Left ventricular ejection fraction.
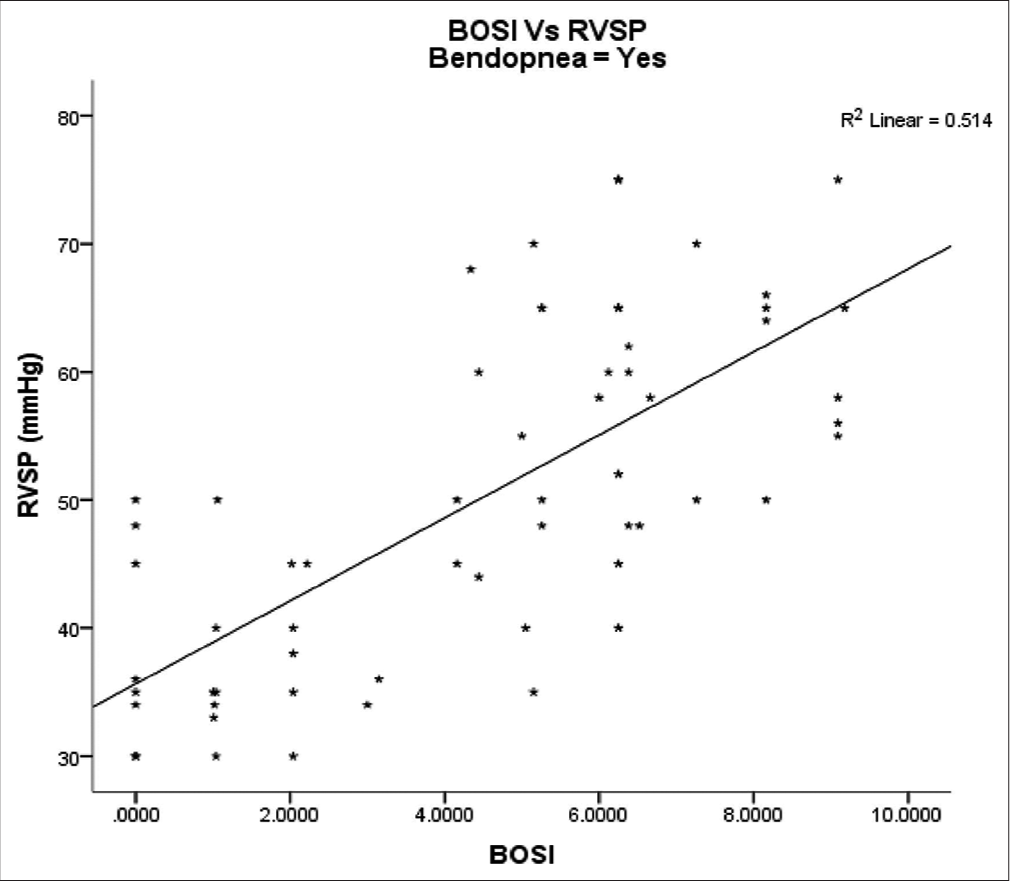
- BOSI versus RVSP in patients with bendopnea. BOSI: Bendopnea saturation index, RVSP: Right ventricular systolic pressure.
There was a negative correlation between BOSI and LVEF, and a positive correlation between BOSI and RVSP.
DISCUSSION
In patients with HF, increased ventricular filling pressures lead to decompensation. The physical examination is essential in the diagnosis and management of patients with HF and can provide an insight into cardiac filling pressures as important as BNP.[6,7] Shortness of breath is the most common symptom of decompensation of HF, but it can also be present in patients with COPD and Asthma. It is a sensitive but not a specific sign of HF. Orthopnea and PND are the most specific symptoms of elevated ventricular filling pressures in HF. A similar worsening of shortness of breath associated with positional change-bendopnea, defined as shortness of breath worsening on bending forward associated with fall in saturation, has been described in the literature[1,2] but not many studied about, and also there were not, many studies about quantification of fall in the saturation on bending forward. In this study, we studied the incidence of bendopnea, its correlation with other clinical findings, echo findings, and an index of fall in saturation-BOSI[8], and its association with short-term prognosis.
This study included slightly more female patients. In patients with bendopnea, there was slight female preponderance when compared to patients without bendopnea, but this difference was not statistically significant.
In this study, bendopnea was present in patients with both preserved and reduced ejection fraction, in contrast to the study of Thibodeau et al. in which bendopnea was present in ∼28% of patients with a mean age of 58 years and decreased LVEF (mean of 20%).[1]
Bendopnea could occur in people without HF, especially in the elderly and in those with higher body mass index (BMI), but this fact has not been studied. The pathophysiology is uncertain.[3] This study did not show any significant association between bendopnea and BMI, possibly because the sample BMI was lower than in previous studies.
We observed that patients with bendopnea had right and left cardiac symptoms, such as orthopnea, PND, oliguria, elevated jugular venous pressure (JVP), and abdominal fullness (abdominal bloating and pressure), similar to findings in previously published studies.[1]
de la Espriella-Juan et al. studied BOSI in ambulatory patients compared with worsening HF events and hospitalizations, which showed BOSI and not bendopnea was independently associated with an increased risk of total (first and recurrent) worsening heart failure (WHF) episodes.[8] In our study, we studied the significance of BOSI in patients admitted with HF, its association with other symptoms of HF, and short-term outcome.
Similar to the previous studies, we found a relationship between bendopnea and PASP, which indicates the severity of pulmonary hypertension, as opposed to LVEF.[3,9,10]
This study focuses on the association between BOSI and echocardiographic measurements. BOSI had a positive association with RVSP and a negative association with LVEF. This shows that BOSI can be useful as a clinical marker for increased filling pressure in patients with HF. BOSI also correlated significantly with short-term mortality. A study recently done by de la Espriella-Juan et al. showed a correlation between BOSI and worsening HF events and hospitalizations.[8] BOSI is a simple bedside index that is proved in this study to be having good use in prognosticating patients admitted with HF.
CONCLUSION
Bendopnea and falling of desaturation on bending are signs of significance in HF patients. The presence of bendopnea correlated with increased pulmonary arterial pressure and with other symptoms of respiratory variation, namely – orthopnea and PND, and higher values of biomarker (NTproBNP). BOSI, but not bendopnea had a significant positive correlation with RVSP and a negative correlation with LVEF. BOSI also correlated with short-term mortality.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Characterization of a novel symptom of advanced heart failure: Bendopnea. JACC Heart Fail. 2014;2:24-31.
- [CrossRef] [PubMed] [Google Scholar]
- "Flexo-dyspnea": A novel clinical observation in the heart failure syndrome. J Heart Lung Transplant. 2013;32:844-5.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of supine posture on airway blood flow and pulmonary function in stable heart failure. Respir Physiol Neurobiol. 2011;178:269-74.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of bendopnea impact on decompensated heart failure. Eur J Heart Fail. 2017;19:111-5.
- [CrossRef] [PubMed] [Google Scholar]
- Bendopnea and risk of adverse clinical outcomes in ambulatory patients with systolic heart failure. Am Heart J. 2017;183:102-7.
- [CrossRef] [PubMed] [Google Scholar]
- The physical examination in heart failure Part II. Congest Heart Fail. 2007;13:99-104.
- [CrossRef] [PubMed] [Google Scholar]
- Bedside assessment of cardiac hemodynamics: The impact of non-invasive testing and examiner experience. Am J Med. 2011;124:1051-7.
- [CrossRef] [PubMed] [Google Scholar]
- Bending oxygen saturation index (BOSI) and Risk of worsening heart failure events in chronic heart failure. Eur J Heart Fail. 2022;24:2108-17.
- [CrossRef] [PubMed] [Google Scholar]
- Bendopnea and its clinical importance in outpatient patients with pulmonary arterial hypertension. Acta Cardiol Sin. 2018;34:518-25.
- [Google Scholar]
- “Bendopnea” or “kamptopnea”? Some thoughts on terminology and mechanisms. JACC Heart Fail. 2014;2:425.
- [CrossRef] [PubMed] [Google Scholar]







